Share this article and save a life!
I am a big technology nerd, I have been one since I was 6 years old and my dad got the first 286 IBM computer in the early 80s. I still remember learning to type, play games, etc. Wow, times have changed.
Early in my childhood, I used to sit in front of my big wooden tv and watch open-heart surgery eating Cheerios. I always wanted to be a doctor early on but realized that my skills in computers surpassed my medical knowledge, so I decided to combine them and build solutions for my friends who worked in healthcare instead.
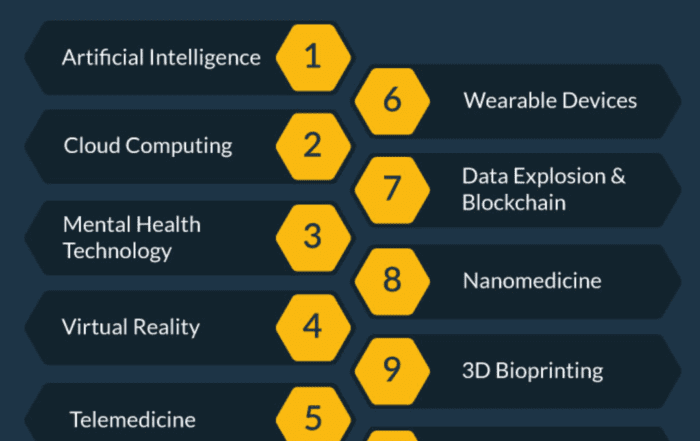
Enough out me, What do I feel are the top healthcare technologies of 2024 and beyond? Continue reading and be inspired.
1. Natural Language Processing (Improved Chat Bots)
Not necessarily the #1 technology, but ChatGPT could offer some exciting new solutions in the future as it matures. So what is ChatGPT and how can it improve healthcare?
ChatGPT is a language model developed by OpenAI. It is a variant of the GPT (Generative Pre-trained Transformer) model, which is a neural network-based machine learning model that has been trained on a large dataset of text. The model can generate natural-sounding text that is similar to human writing. ChatGPT is specifically trained to generate conversational text. This means that it can understand and respond to prompts in a way that mimics a human conversation. This makes it useful for tasks such as chatbot development, language translation, and text summarization.
ChatGPT can be used to assist with a variety of tasks in healthcare such as natural language processing, automated medical coding, and virtual assistants for patients. Additionally, it can be used to generate personalized medical reports, assist with drug discovery and clinical trial matching, and help with clinical decision support.
However, it is important to note that GPT is a model trained on text data and has not been specifically trained on healthcare data, so it may not be fully accurate or reliable in certain healthcare applications.
Explore the perspective of a physician regarding ChatGPT.
Gregory Jasani M.D., an EM doctor in Maryland, recently wrote about his experiences using ChatGPT in an article called, “A Doctor’s First Impressions of ChatGPT: Is it a Game-Changer for the Future of Healthcare?” It is worth a read.
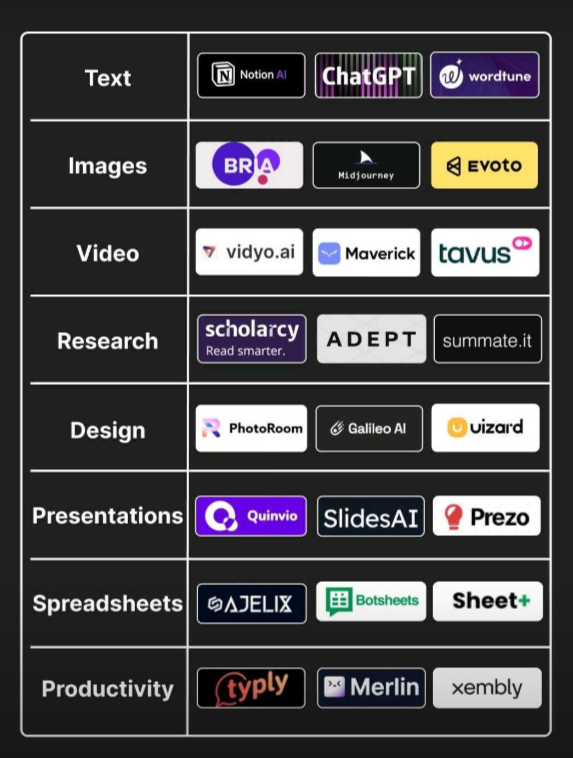
A few AI tools that may be useful:
2. Chronic Disease Management Software
Healthcare services can only be effective if patients have access to them. Unfortunately, healthcare inequalities and social determinants of health (SDOH) can prevent patients from accessing these services. In recent years, there has been an increased focus on tracking the patient journey and identifying the reasons why some individuals do not use available resources, even when they are covered by Medicare.
Some examples of SDOH include:
- Income and social protection
- Education
- Unemployment and job insecurity
- Working life conditions
- Food insecurity
- Housing, basic amenities, and the environment
- Early childhood development
- Social inclusion and non-discrimination
- Structural conflict
- Access to affordable health services of decent quality
Caremessage.org, founded in 2012 by Vineet Singal, is a great solution for FQHCs. They help safety net organizations be more efficient with their time, and increase the quality of care and health outcomes for their patients across the health journey.
Another company we like that is starting to gain traction is Pear Suite a company founded by Colby Takeda. They are laser-focused on building the best social care navigation software for health and community organizations. They address the social determinants of health that greatly impact older adults and underserved populations.
3. Applying AI to Preventative Cancer Care
To start AI has been a dirty word in healthcare for a while now, it has been all promises and many failures. See a recent article I wrote “The Truth about Healthcare AI and why it has Failed so Far” to see why this is the case.
The largest challenge has been reimbursement. lead by CMS. Very few companies have products or services that are reimbursable using computer vision or machine learning solutions. If a clinic can not get paid for services, it will not invest the time, or resources to build technology. Even if it was reimbursed, most clinics could not afford to build or manage a tech solution, so they will require partnerships to bring these technologies to light.
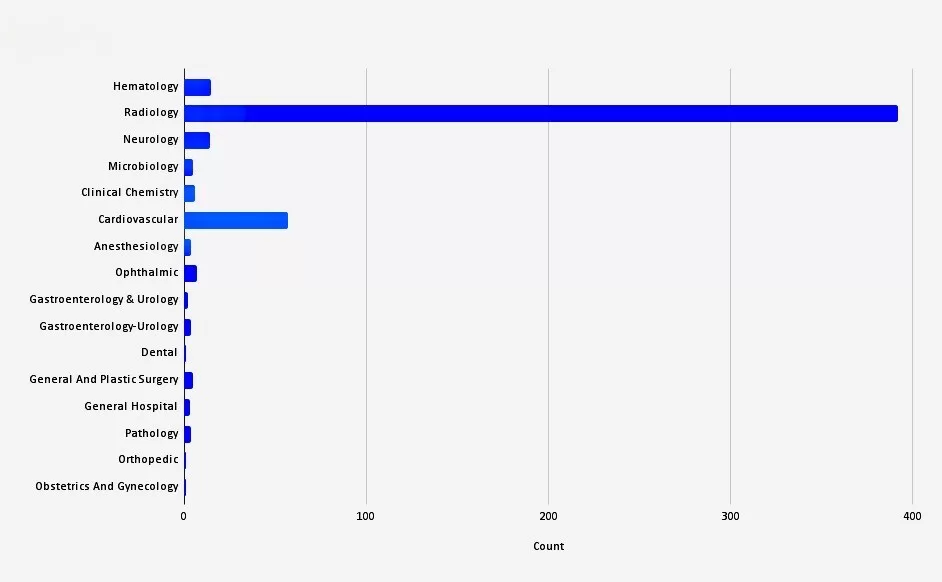
For example, there are over 500 AI-enabled solutions with the vast majority in the Radiology space and almost all of them are not reimbursable by Medicare, which limits their use.
So what is changing, Medicare and Commercial Insurers are now finally stepping up to the plate and offering reimbursement for new computer vision solutions that can screen for cancer and provide a risk analysis of a nodule.
Radiology + Primary Care = #EarlyDetection
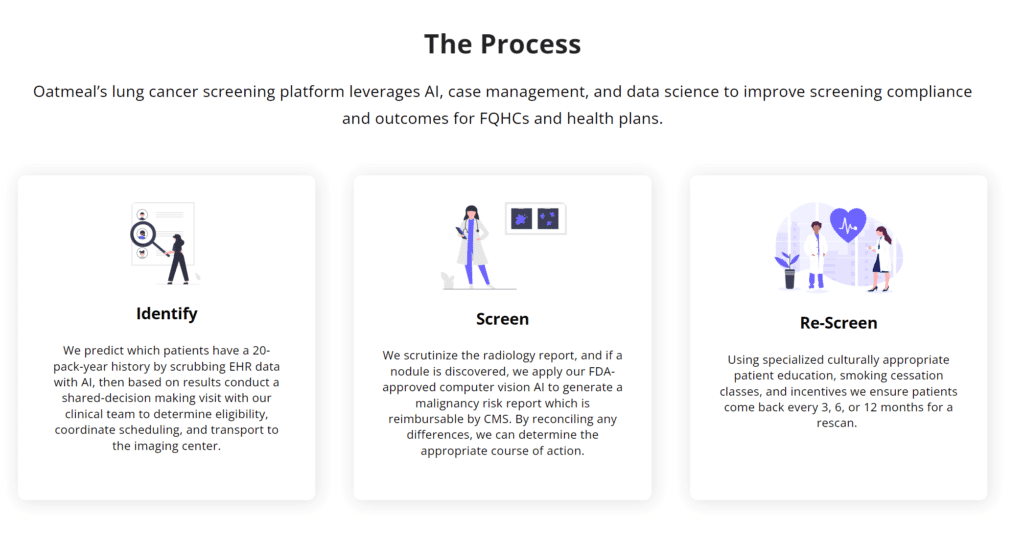
New startups like OatmealHealth.com, are incorporating AI into clinical workflows and partnering with FQHCs and health plans to preventatively screen high-risk patients for cancer, starting with lung and expanding to other disease states in the future including breast, prostate, and colorectal. This is a massive change to how cancer is screened and will help provide better access and education to underserved patients who need it most. By combining engagement solutions and identifying social determinants that prevent patients from attending appointments,
Oatmeal Health guides patients through their entire journey from identification using machine learning to helping them find rides to their appointments all in one call. The patients do not have to call 5 to 10 different facilities to figure out how to get help, Oatmeal does all the work for them and does not make the clinic add another to-do item to their busy day.
Why is it important: Lung cancer is a serious national problem, it takes more lives annually in the U.S. than the next three deadliest cancers combined, breast, prostate, and pancreatic
- When diagnosed early, the survival rate is high for lung cancer – 92%
-
When diagnosed late, the survival rate is low for lung cancer – 3.5%
4. Robotic Surgery for Minimally Invasive Procedures
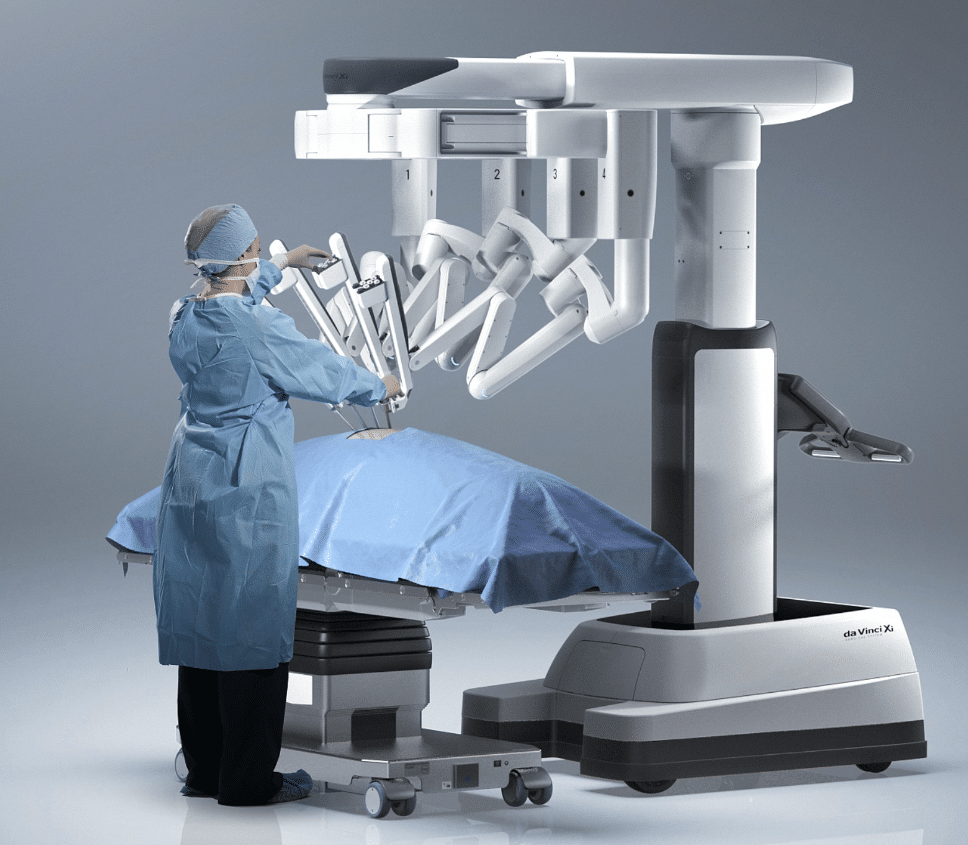
Robotic surgery for minimally invasive procedures can help healthcare by providing surgeons with more precision and control during the procedure, which can lead to improved outcomes for patients. Additionally, because the incisions used in robotic surgery are smaller than those used in traditional open surgery, patients may experience less pain and scarring and have a quicker recovery time. Robotic surgery can also be less invasive than traditional open surgery and may be used in cases where traditional surgery would not be possible. This can allow for earlier intervention and treatment of certain conditions, which can improve patient outcomes.
Intuitive remains the dominant surgical robotics company, but corporations ranging from Medtronic to Vicarious Surgical look to compete. Intuitive is best known for its da Vinci surgical robotics system. But there is a buzz around its Ion system, with its fully articulating catheter making its way through the lungs for cancer biopsy. Watch out for even more from Ion down the road. For example, Intuitive has obtained German regulatory approval for a clinical study of Ion ablation technology.
During a keynote interview at October’s DeviceTalks West in Santa Clara, California, Guthart said there could be even further opportunities for Ion technology down the road:
“It opens up opportunities for tubular structures outside the lung as well. I think over time, that opportunity will grow.”
5. Quantum Computing for Drug Discovery
Quantum computing has the potential to significantly accelerate drug discovery by enabling the simulation of complex chemical systems and the analysis of large amounts of data. This can help researchers identify new drug candidates and optimize existing ones more quickly and efficiently.
One of the main advantages of quantum computing is its ability to perform certain calculations much faster than classical computers. This is particularly useful in the field of drug discovery, where simulating the behavior of complex molecules and predicting their interactions with proteins can be computationally intensive. Quantum computers can also help to analyze large amounts of data from experiments and clinical trials, which can provide insights into the underlying biology of disease and aid in the discovery of new targets for drug development.
One company I have been following is Qubit Pharmaceuticals. Qubit is building a drug discovery platform using the NVIDIA QODA programming model for hybrid quantum-classical computers and the startup’s Atlas software suite. Atlas creates detailed simulations of physical molecules, accelerating calculations by a factor of 100,000 compared to traditional research methods.
6. Genomics for Understanding Genetic Factors in Disease
Genomics can help healthcare understand genetic factors in disease by allowing for the identification of specific genetic variations associated with a particular disease. This can be done through techniques such as genome-wide association studies (GWAS) and whole genome sequencing.
GWAS involves comparing the genomes of individuals with a particular disease to those without the disease to identify genetic variations that are more common in individuals with the disease. These variations may increase the risk of developing the disease or influence the severity of the disease.
Illumina has been in the news a lot lately for their Cancer Genomics Research and their partnership with Amgen. Illumina’s next-generation sequencing (NGS) and microarray technologies represent the gold standard in quality worldwide—and account for ~90% of the world’s sequencing data.
7. Digital Therapeutics for Treatment of Mental Health Disorders
Large unmet needs in mental health combined with the stress caused by pandemic mitigation measures have accelerated the use of digital mental health apps and software-based solutions.
Digital therapeutics for mental health can help healthcare in several ways:
- Access to treatment: Digital therapeutics can make mental health treatments more accessible to individuals, particularly those in remote or underserved areas, who may not have access to in-person therapy or psychiatrists.
- Convenience: Digital therapeutics can be delivered through smartphones, tablets, or computers, which allows individuals to access treatment at their convenience, and can also be used as an adjunct to in-person therapy.
- Scalability: Digital therapeutics can be delivered to a large number of individuals simultaneously, which can help to address the shortage of mental health professionals and improve access to treatment.
- Cost-effective: Digital therapeutics can be more cost-effective than traditional in-person therapy and can help to reduce healthcare costs.
- Evidence-based: Digital therapeutics for mental health are based on cognitive-behavioral therapy (CBT) and other evidence-based techniques. This allows for a personalized approach to treatment and can improve outcomes for patients.
- Continuous Care: Digital therapeutics can provide continuous care for patients, which can help to prevent relapses and improve long-term outcomes.
Global investor funding for virtual behavioral services and mental health apps in 2021 exceeded $5.5 billion, a 139% jump from 2020, according to CB Insights.
One study of 93 non-FDA approved Android apps (median installs 100,000), targeting mental well-being, found the median 15 and 30-day retention rates were very low at 3.9% and 3.3%. In that study, the daily active user rate (median open rate) was only 4.0%. These data highlight that the number of app installs has very little correlation with daily long-term usage.
So who is doing it right? Lyra Health a Global Workforce Mental Health Service, raised a whopping $900M in funding to make it easier to find and get treatment and use technology to make it smarter, more personalized, and more effective. Lyra uses validated clinical measures, such as the PHQ-9 and the GAD-7, to assess symptom improvement for anxiety, depression, and other common mental health issues. Reliable clinical change is a 6-point difference on the PHQ-9 and a 4-point change on the GAD-7.
8. Augmented Reality (AR) for Medical Education and Surgical Planning
Augmented reality is starting to gain traction in the education field, albeit very slowly due to the poorly designed “apps” of the past. The education sector is forecast to spend more than $6 billion annually on augmented and virtual reality technologies by 2023. Funding for the technologies remains a major hurdle to adoption, but price points for equipment are dropping rapidly, according to a new market forecast from ABI Research.
Medical schools and healthcare institutions are implementing AR, VR, and XR training to enable repeatable immersive surgical simulations that bring valuable practice. Here are some examples.
- The Johns Hopkins School of Nursing has implemented VR training at all levels, from doctoral to prelicensure nursing, according to Kristen Brown, assistant professor at the Johns Hopkins School of Nursing and the simulation strategic projects lead at the Johns Hopkins Medicine Simulation Center. Areas of focus for training include resuscitation, anaphylactic reactions, postsurgical management, acute-care management, and pediatric critical care.
- Dr. Augustus D. Mazzocca, chief of the division of sports medicine at Massachusetts General Hospital, medical director at Mass General Brigham Sports Medicine, and faculty member at Harvard Medical School, uses a system called PrecisionOS to augment orthopedic education. Mass General’s Department of Orthopedic Surgery is also beginning to use PrecisionOS to train medical students and residents in motor skills required for surgery.
- The University of Central Florida College of Nursing implemented AR and VR for nurses and nurse practitioners over the past year, says Mindi Anderson, interim associate dean for simulation and immersive learning and director of the school’s healthcare simulation graduate program.
9. Bioprinting for Tissue Engineering
Bioprinting for tissue engineering can help healthcare by allowing scientists and doctors to create replacement tissues and organs for patients using a patient’s own cells. This can help to reduce the risk of rejection and improve recovery time. Additionally, bioprinting can be used to create 3D models of diseased tissues and organs, which can be used for research and drug development.
One company, Organovo raised $112M to create functional human tissues using proprietary three-dimensional bioprinting technology. Their goal is to build living human tissues that are proven to function like native tissues. With reproducible 3D tissues that accurately represent human biology, they are enabling ground-breaking therapies like bioprinted pluripotent stem-cell-directed kidney organoids.
10. Advanced Imaging Techniques such as MRI, PET, and CT Scans
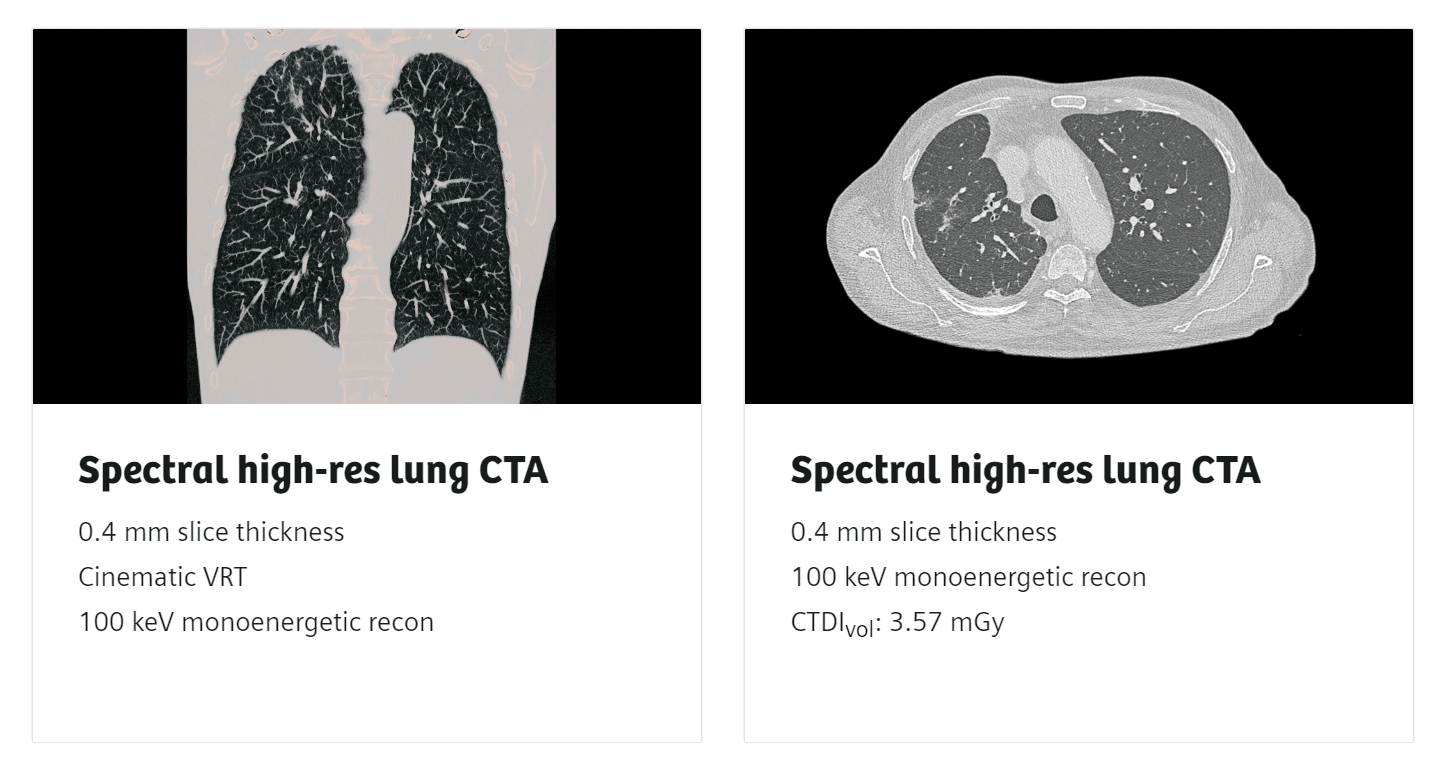
Advances in CT scans hit a major milestone in the last few years with the FDA clearing the first major imaging device advancement for Computer Tomography in nearly a decade.
“Computed tomography is an important medical imaging tool that can aid in diagnosing disease, trauma or abnormality; planning and guiding interventional or therapeutic procedures; and monitoring the effectiveness of certain therapies,” said Laurel Burk, Ph.D., assistant director of the Diagnostic X-ray Systems Team in the FDA’s Center for Devices and Radiological Health. “Today’s action represents the first major new technology for computed tomography imaging in nearly a decade and underscores the FDA’s efforts to encourage innovation in areas of scientific and diagnostic progress.”
The device from Siemens coined Naeotom Alpha uses the emerging CT technology of photon-counting detectors which can measure each X-ray that passes through a patient’s body, as opposed to current systems which use detectors that measure the total energy contained in many X-rays at once. By ‘counting’ each X-ray photon, more detailed information about the patient can be obtained and used to create images with less information that is not useful in the review and analysis.
NAEOTOM Alpha offers an easy and streamlined way to get quantitative information in addition to morphology. By matching the appropriate protocols to patients and by combining all necessary acquisitions into a single scan, NAEOTOM Alpha enables smart navigation through the diagnostic pathway.
11. Microfluidics for lab-on-a-chip applications
Microfluidics, or the manipulation of fluids at the microscale, is useful for lab-on-a-chip applications in healthcare because it allows for the integration of multiple laboratory processes onto a small, portable device. This can greatly increase the efficiency, speed, and accuracy of diagnostics, as well as reduce the cost and complexity of laboratory testing.
Additionally, microfluidic devices can be designed to mimic the physiological microenvironment of cells, which can be useful for studying the behavior of cells in the human body and developing new treatments. Overall, microfluidics technology has a lot of potential to improve healthcare by making laboratory testing more accessible, efficient, and effective.
Here is a short list of companies that have some interesting products coming out in 2023 and beyond.
- Standard Biotools (formerly Fluidigm) – The company has raised over $60 million in funding according to Crunchbase before the acquisition.
- Bio-Rad Laboratories – The company has raised over $100 million in funding according to Crunchbase.
- Beckman Coulter (Formerly Labcyte) – The company raised over $100 million in funding according to Crunchbase before the acquisition.
It is worth noting that in the field of microfluidics, there are also many research institutions, universities, and government organizations that receive funding for microfluidics research.
12. Synthetic Biology for Gene Therapy
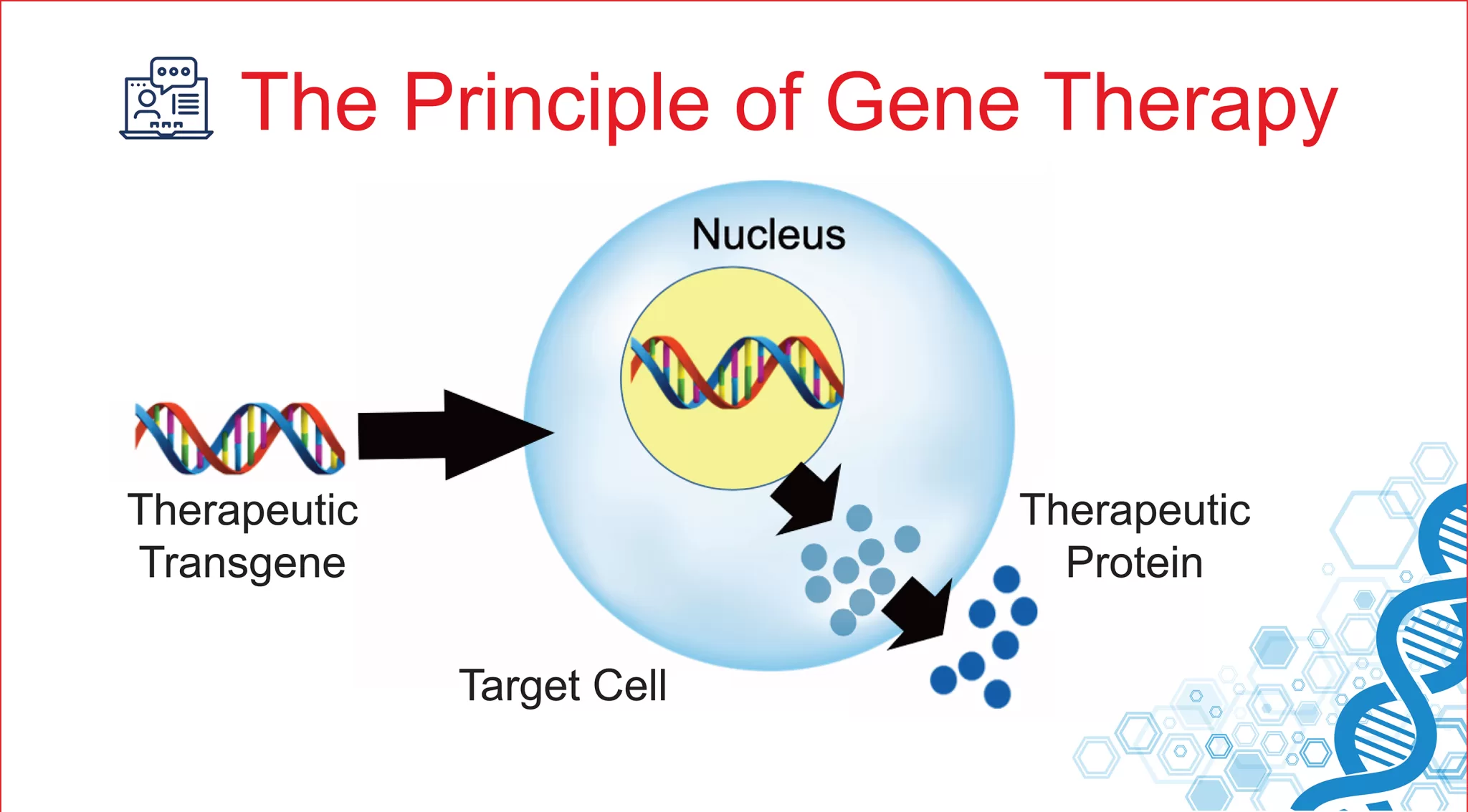
Synthetic biology, which involves the design and engineering of biological systems, has a lot of potential value for healthcare, particularly in the field of gene therapy. Gene therapy is a treatment approach that involves the delivery of functional genes to cells in the body to correct genetic disorders. Synthetic biology can be used to design and engineer new genetic constructs that can be used for gene therapy, including viral vectors, which are used to deliver therapeutic genes to target cells.
One of the main advantages of synthetic biology for gene therapy is the ability to precisely control the expression of therapeutic genes. Synthetic biology techniques can be used to create genetic constructs that only express therapeutic genes in specific cell types or under specific conditions, reducing the potential for off-target effects.
Additionally, synthetic biology can be used to create new genetic tools and platforms that are more efficient and effective at delivering therapeutic genes to target cells. Synthetic biology can also be used to create new gene editing tools, such as CRISPR, that can be used to precisely and efficiently correct genetic disorders at the DNA level.
Overall, synthetic biology has a lot of potential to improve healthcare by advancing the field of gene therapy, allowing for the development of more precise, targeted, and effective treatments for genetic disorders.
One of the most funded companies, Intellia Therapeutics raised upwards of 1.2B dollars.
They are focused on the development of curative therapeutics utilizing a recently developed biological tool known as the CRISPR/Cas9 system. We believe that CRISPR/Cas9 technology has the potential to transform medicine by permanently editing diseased genes in the human body through a single treatment course.
13. Stem Cell Therapy for Regenerative Medicine
Stem cell therapy is important in healthcare because it has the potential to revolutionize regenerative medicine. Stem cells are a unique type of cell that has the ability to develop into many different cell types in the body, including cells of the blood, skin, heart, and brain. This ability makes stem cells an attractive option for regenerative medicine, which aims to replace or repair damaged or diseased cells, tissue, or organs.
One of the main advantages of stem cell therapy for regenerative medicine is the ability to repair or replace damaged or diseased cells and tissue with healthy, functional cells. This can be achieved by transplanting stem cells into the body, where they can develop into the cells that are needed to repair or replace damaged tissue. This can be used to treat a wide variety of conditions, including injuries, diseases, and genetic disorders.
One of the most well-funded Stem Cell companies is Fate Therapeutics which has raised $1.2B. They are a stem cell and developmental biology research company using biological mechanisms to develop stem cell therapeutics.
14. Wearable Technology for Monitoring Vital Signs and Activity Levels
Wearable technology will be the top global fitness trend in 2023, according to the American College of Sports Medicine (ACSM), which released on Dec. 28 results from its annual international survey of 4,500 health and fitness professionals.
The survey asked fitness professionals from around the world to assess 42 potential trends, and 20 of the top trends were detailed in a report by ACSM. In addition, ACSM broke down trends for various countries, including the United States where wearable technology also came in as the No. 1 trend in 2023.
“Wearables are certainly not going anywhere,” ACSM Past President Walter R. Thompson, who served as the lead author of the survey, said in the media release. “Not only are these devices becoming more affordable, but wearable data is increasingly being used in clinical decision making so they are continuing to hold their appeal.”
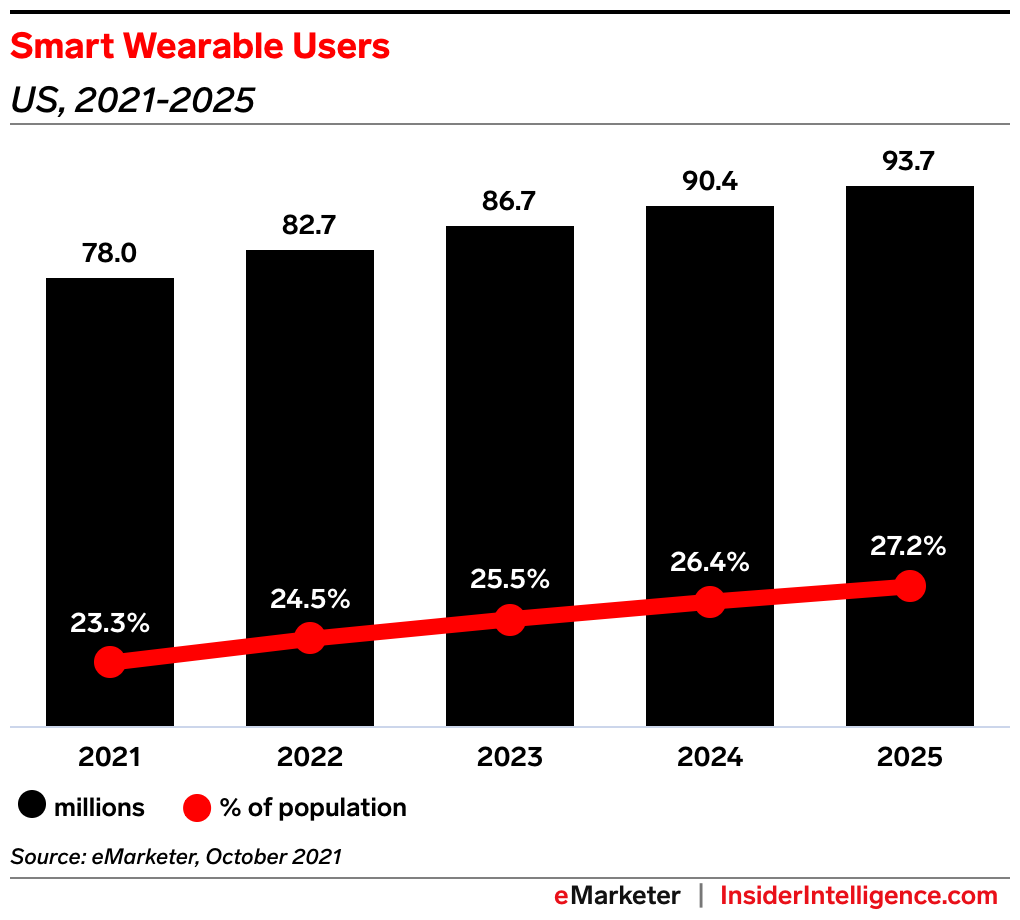
Demand for wearables is expected to continue to rise in the next few years, as consumers exhibit interest in sharing their health data with providers and insurers. The US Smart wearable user market is poised to grow 25.5% YoY in 2023, up from 23.3% YoY growth in 2021, per an October 2021 forecast by Insider Intelligence.
The Fitbit Flex was an early, popular option for wearable technology consumers. Users were attracted to its sleek look and ability to track their step progress throughout the day with the device’s five indicator lights. Its most recent iteration, the Fitbit Sense 2, offers an array of health-tracking features to improve sleep and eliminate, and battery life that can last a full week.
The latest rumors claim that Apple will announce the Reality Pro headset soon, possibly during a spring Apple event. Apple may allow developers to test the headset and begin coding apps for it in June when the Worldwide Developers Conference (WWDC) is expected to take place.
Reports suggest that the first iteration of the headset might have issues, including the need for a large, waist-mounted battery pack. If that’s the case, quirks such as that coupled with the expected $3,000+ price might make the first-generation model one to miss.
15. Blockchain for Secure Medical Data Storage
Blockchain technology can help secure medical data storage by providing tamper-proof and decentralized record keeping. This means that once data is entered into the blockchain, it cannot be altered or deleted, providing a permanent and secure record of the patient’s information. Additionally, because the data is decentralized and stored on multiple nodes, it is less vulnerable to hacking or data breaches.
Doctors can benefit from this secure data storage by having access to a patient’s complete and accurate medical history, which can help inform diagnosis and treatment decisions. Additionally, because the data is stored on a secure and decentralized network, doctors can be more confident that their patients’ sensitive information will not be compromised.
There are a number of companies that are currently exploring or implementing blockchain technology for healthcare data management. Some examples include:
- BurstIQ is a Web3-ready blockchain platform that manages and secures data
- Guardtime is a company that uses blockchain technology to secure medical data, including EHRs and medical images.
These are just a few examples and the list of companies working in this area is growing.
Older video but still applicable.
16. Nanotechnology for Targeted Drug Delivery
Nanotechnology refers to the manipulation and engineering of materials at the nanometer scale (typically between 1 and 100 nanometers in size). This technology can be used in targeted drug delivery, which refers to delivering drugs to specific cells or tissues in the body.
Nanoparticles, which are particles that are between 1 and 100 nanometers in size, are one example of how nanotechnology can be used for targeted drug delivery. These particles can be engineered to carry drugs directly to cancer cells while leaving healthy cells unharmed. Additionally, nanoparticles can also be designed to evade the body’s immune system, allowing drugs to reach their target more effectively.
Another example is the use of liposomes, which are spherical structures composed of a phospholipid bilayer and can be used to encapsulate drugs and target them to specific cells or tissues in the body.
Overall, the field of nanotechnology for targeted drug delivery is an active area of research, and it holds great promise for improving the effectiveness and safety of drug treatments. However, more research and development is needed before these technologies are used in clinical practice.
Key Market Players
Product launches, mergers and acquisitions, joint ventures, and geographical expansions are key strategies adopted by players in the Nanotechnology Drug Delivery Industry. The top 10 companies in the Nanotechnology Drug Delivery Market are:
- Taiwan Liposome Company
- NanOlogy LLC
- Nanobiotix
- Aquanova AG
- NanoCarrier Co Ltd
- Novartis International AG
- Calgene Corporation
- Amgen Inc
- Merck and Co.
- Johnson & Johnson Private Limited
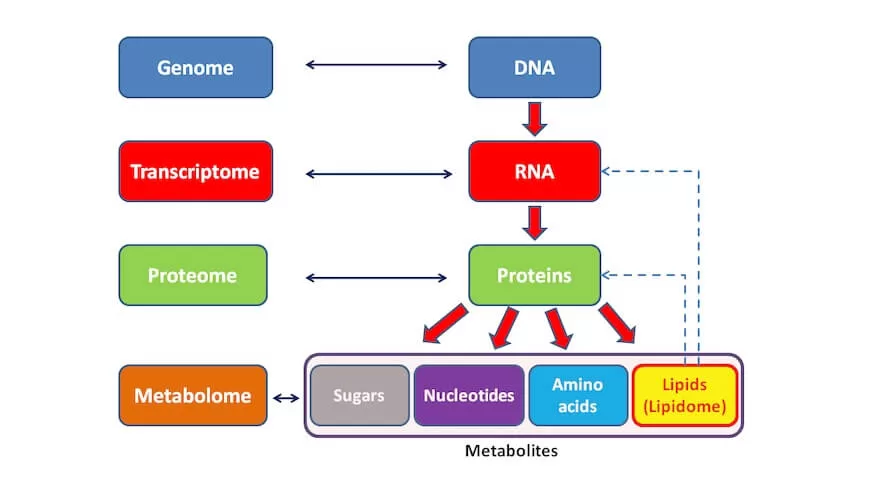
17. Metabolomics for Disease Diagnosis
Metabolomics is the study of the metabolites in an organism, which are the small molecules that are involved in metabolism. It can be used for disease diagnosis by analyzing the metabolic profile of a patient’s blood, urine, or other biofluids.
By analyzing the levels of different metabolites, researchers can gain insight into the metabolic changes that occur in a patient’s body as a result of a disease. This information can then be used to help diagnose the disease and to monitor the effectiveness of treatment.
One of the major benefits of metabolomics for disease diagnosis is that it can help to identify diseases earlier and more accurately than traditional diagnostic methods. For example, changes in the metabolic profile of a patient’s blood may be one of the earliest signs of a disease, such as cancer, long before symptoms appear.
Additionally, because metabolomics can provide a holistic view of the metabolic changes that occur in a patient’s body, it can help to identify multiple diseases simultaneously, which can save time and resources in the diagnostic process.
Metabolomics is also a relatively non-invasive diagnostic method, which can reduce the risk and discomfort of diagnostic procedures for patients.
Overall, metabolomics has the potential to change healthcare by providing a new way to diagnose diseases, earlier and more accurately, which can lead to more effective treatments and better outcomes for patients.
- Metabolon: A company that provides metabolomics services and technology, including sample preparation, analytical services, and software for data analysis.
- Biocrates Life Sciences: A company that specializes in targeted metabolomics, which is a method of analyzing specific metabolic pathways or classes of compounds.
- LECO Corporation: A company that provides analytical instruments and software for metabolomics research.
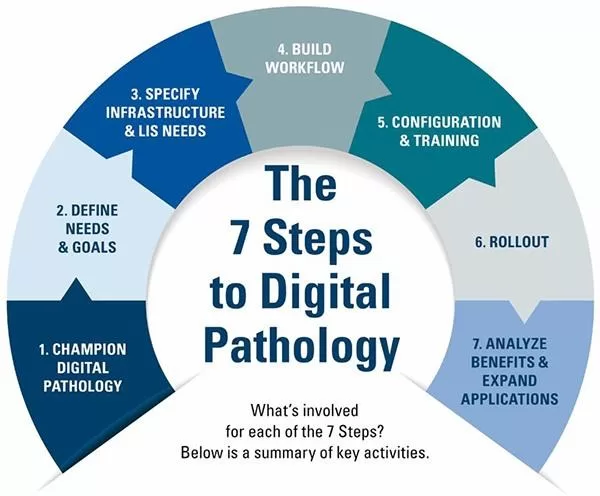
18. Digital Pathology for Faster and More Accurate Diagnoses
Digital pathology refers to the use of digital technology to analyze and interpret pathology images, such as those taken from biopsies or other tissue samples. This technology can be used to create digital images of pathology slides, which can then be viewed, analyzed, and shared electronically.
Digital pathology can help doctors in several ways:
- Speed: Digital pathology allows for faster diagnoses because digital images can be analyzed and interpreted quickly, even remotely.
- Precision: Digital pathology can provide higher precision in diagnoses because the images can be enlarged and manipulated for a more detailed view of the tissue.
- Remote consultation: Digital pathology images can be easily shared with other pathologists or specialists for a second opinion, which can be done remotely, which can save time and resources, and also provide a wider range of expertise to the diagnosis process.
- Automated analysis: Digital pathology can be used in conjunction with machine learning algorithms, which can help to automate the analysis of pathology images and make the process more objective and consistent.
- Archiving: Digital pathology allows for easy archiving of pathology images, which can be accessed and reviewed later, and can be helpful in tracking the patient’s medical history.
Overall, digital pathology has the potential to improve the diagnostic process by providing faster and more accurate diagnoses, which can lead to more effective treatments and better outcomes for patients.
- Aiforia‘s cloud-based products and services are designed to decrease the burdens experienced by pathologists due to outdated equipment. Aiforia also aims to reduce wait times for patients and create more reliable treatments by providing them with accurate diagnoses and treatment plans.
- Deep Bio, Based in South Korea, Deep Bio has the goal of driving innovation in technology, providing clinicians with the tools to make critical decisions and improve patient outcomes. They recognize the gap between pathologists based on their areas of experience that is causing inconsistencies in diagnoses and are working to bridge that gap with artificial intelligence. Their AI is a deep learning-based cancer diagnostic support software that is designed to unlock personalized insights for clinicians and strengthen healthcare delivery to support both clinicians and patients.
19. Circadian Health
Circadian health refers to the alignment of an individual’s biological rhythms with the natural light-dark cycle of the environment. This includes maintaining regular sleep patterns, exposure to natural light during the day, and avoiding artificial light at night.
Circadian health can have a positive impact on healthcare in several ways. For example, it can:
- Improve sleep quality and duration, which can lead to better overall health and a reduced risk of sleep-related disorders such as insomnia and sleep apnea
- Regulate the body’s production of hormones and neurotransmitters, which can help to improve mood and cognitive function
- Reduce the risk of chronic diseases such as diabetes, heart disease, and cancer by regulating metabolism and inflammation
- Improve the effectiveness of certain medications and treatments by timing them to align with the body’s natural rhythms
- Improve the outcomes of certain medical procedures by scheduling them during times when the body is better able to handle the stress of surgery or recovery.
Additionally, it’s also been found that the alignment of our circadian rhythm with the natural light-dark cycle can prevent or alleviate some mental health disorders such as depression, bipolar disorder, and seasonal affective disorder (SAD).
Last August, Rebecca Robbins, who holds a doctorate in communication and health marketing, collaborated with the bio alarm clock app Sleep Cycle to release a report on the state of sleeplessness during the pandemic. In it, researchers aimed to see how the pandemic affected sleep and mental health.
Some key findings included that teens and young adults had the worst quality sleep, and reported the highest rates of depression; women were twice as likely to report taking longer to fall asleep than men; and 45 percent of respondents reported heightened anxiety while 24 percent reported heightened feelings of depression.
“Sleep is a fascinating part of the day, and we have to do it or there are consequences,” said Robbins, who is associate scientist at Brigham and Women’s Hospital and instructor in medicine at Harvard Medical School. “We are irritable, anxious and make poor decisions in other areas of health, like appetite and exercise.”
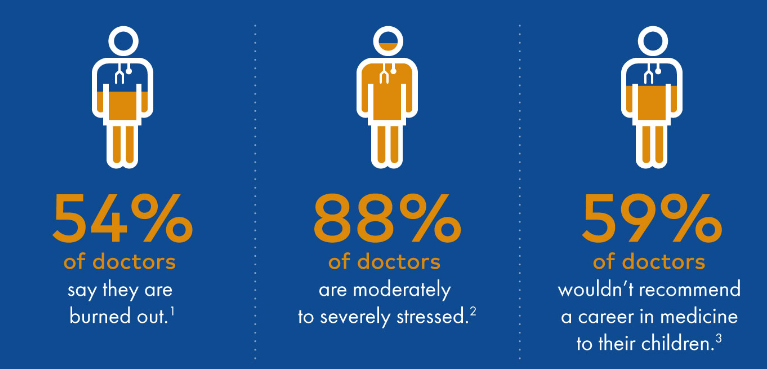
20. Focus on Clinician Burnout
Clinician burnout is a significant issue in the healthcare industry and it can have a negative impact on both doctors and their patients. Some of the common causes of burnout among clinicians include:
- High workload and long working hours
- Lack of control over work-life balance
- Inadequate support from colleagues and supervisors
Fortunately, these startups have discovered ways to employ technology to begin to fix this lopsided system. Meet the companies that are using augmented intelligence and digital platforms that consumers use daily to improve healthcare organizations’ baseline understanding of the challenges to clinician well-being.
- Robert Stern, founder, and CEO of @Point of Care (@POC), is on a mission to deliver quality care to every patient by giving clinicians access to the right information, at the right time.
- Kim Kristiansen and JG Staal, co-founders of Zignifica, are passionate about taking evidence-based medicine to the next level. What does that look like? Finding the most trustworthy information presented in medical papers, and making that information available for those who need it most — patients, their relatives, and healthcare professionals.
- For Eran Kabakov, CEO of Docola, transforming doctor-patient communication is all about less repeating and more treating. The company’s responsive web platform collects content from a provider’s computer, mobile phone, YouTube, or Docola’s integrated patient education marketplace, combines content into courses to “prescribe” to patients, and allows providers to collect participation data in order to optimize clinical and business workflows.
Several strategies can be implemented to help reduce clinician burnout:
- Increase support from colleagues and supervisors: Clinicians should be provided with regular opportunities to connect with colleagues, and supervisors should be available to provide guidance and support when needed.
- Provide access to mental health support: Clinicians should be provided with access to mental health support services and counseling, as well as opportunities to debrief after traumatic or emotionally distressing events.
- Implement team-based care and shared decision-making: Clinicians should be encouraged to work in teams and be involved in shared decision-making, as it can reduce their workload and improve their sense of autonomy.
21. Patient Engagement Solutions
Patient engagement solutions are technologies or strategies that are designed to promote active participation and collaboration between patients and healthcare providers. They are increasingly important because they can help to improve the quality of care, increase patient satisfaction, and reduce healthcare costs.
We mentioned OatmealHealth.com, and Caremessage.org for the FQHC market, but here are a few other segments to review.
- Electronic health records (EHRs) allow patients to access their health information, communicate with their healthcare providers, and schedule appointments.
- Patient portals provide patients with access to their health records, lab results, and other information.
- Telemedicine platforms allow patients to connect with healthcare providers remotely.
- Wearable devices that allow patients to track their health data and share it with their healthcare providers.
- Patient education and self-management tools provide patients with the information and resources they need to manage their own health.
Here are a few other companies to watch.
- Solutionreach.
- RevenueWell.
- OhMD.
- Updox.
- Artera.
- Pabau.
- MyChart.
- PatientPop, a Tebra Company.
In summary, patient engagement solutions are important because they provide patients with the tools and resources they need to manage their own health, which can lead to better health outcomes, improved patient satisfaction, and reduced healthcare costs.
22. Increase Utilization of Telemedicine
Telemedicine is the use of telecommunication and information technologies to provide healthcare services remotely. It has become increasingly popular in recent years due to its ability to provide patients with access to healthcare services regardless of location, which can have many benefits. Some of the benefits of telemedicine include:
- Better management of chronic conditions: Telemedicine can help improve the management of chronic conditions by providing patients with the tools and resources they need to monitor their own health, and communicate with healthcare providers when needed.
- Improved continuity of care: Telemedicine can help to improve continuity of care by allowing patients to stay connected to their healthcare providers even when they’re not able to come into the office.
- Increased patient engagement: Telemedicine can help to increase patient engagement by providing patients with more opportunities to communicate with their healthcare providers.
The key with anything is education and access, by taking the time out of a standard primary care engagement to teach patients about how to use telemedicine we will see improvements in overall health in the long run. The challenge is that most primary care physicians only have 15 minutes with a patient or less, so there is not much time to provide this education as noted in the article “The Battle Between Primary Care and Time: The Doctors are Losing”.
Overall, increasing the use of telemedicine requires a multifaceted approach that includes making it easy to use, providing education and training, increasing awareness and reimbursement, implementing regulations and standards, improving technology and infrastructure, creating partnerships and collaborations, addressing barriers, encouraging the use in certain situations, and monitoring and evaluating the service.
- Teladoc.
- MeMD.
- HealthTap.
- Amwell.
- MDLive.
- Doctor on Demand.
- LiveHealth Online.
- Virtuwell.
23. Smart Implants
Smart implants are medical devices that are implanted in the body and can communicate with external devices to provide real-time monitoring and treatment of medical conditions. They are helping patients by:
- Improving the management of chronic conditions: Smart implants can be used to monitor and treat chronic conditions such as diabetes, heart disease, and Parkinson’s disease. For example, a smart insulin pump can automatically adjust insulin levels in response to continuous glucose monitoring.
- Reducing the need for invasive procedures: Smart implants can be used to deliver medication and other therapies directly to the site of an injury or illness, reducing the need for invasive procedures such as surgery.
- Improving the quality of life for patients: Smart implants can help to improve the quality of life for patients by providing more effective treatment, reducing the need for frequent hospital visits, and allowing patients to more easily manage their health.
- Remote monitoring: Smart implants can be connected to remote monitoring systems, allowing healthcare providers to monitor patients remotely, and provide care and support as needed.
Competitive Landscape
The smart implant devices market is consolidated in nature due to the presence of few companies operating globally as well as regionally. The major market players are focusing on technological advancements to acquire maximum market share. Some of the Major Players include Stryker, Zimmer Biomet, DePuy Synthes, Medtronic, IQ Implants USA, Canary Medical Inc., NuVasive Inc. Smart Implant Solutions, REJOINT SRL, among others.
North America is expected to dominate the market owing to factors such as the easy availability of technologically advanced products, high awareness among consumers, improved healthcare infrastructure, and expansion of pharmaceutical and biotechnology companies in the region. For instance, according to data provided by Stanford Children’s Health Organization, Sports Injury statistics,
In 2021, 30 million children and teens will participate in some form of organized sports, and more than 3.5 million will have injuries each year in the United States. An increase in the usage of smart implants for rapid and effective results in the United States is among the key factors that contribute to the growth of the studied market in North America.
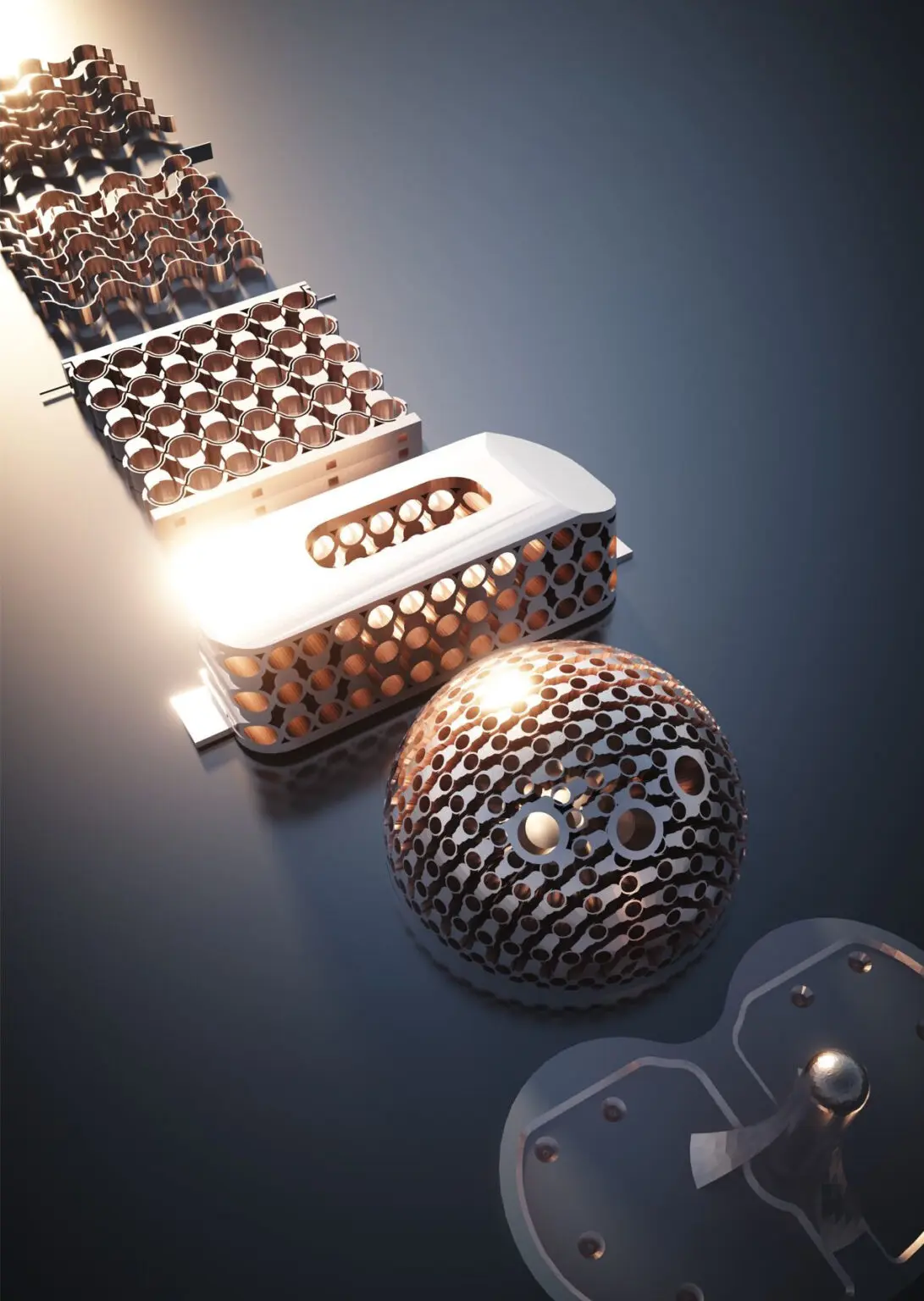
An illustration of potential smart implants using the advanced metamaterial developed by the iSMaRT Lab at the University of Pittsburgh.
A team of researchers at the University of Pittsburgh’s Swanson School of Engineering recently announced the development of a patient-specific, 3D-printed, smart metamaterial spine implant. The device leverages highly sophisticated technologies to double as a self-powered sensor that monitors bone healing in the spine. Their findings were published in the Advanced Functional Materials journal.
“This is clinically significant because surgeons can use the data generated by the implants to directly and precisely assess the bone healing progress,” Dr. Alavi said. “These features can potentially eliminate the need for radiographic imaging techniques, which are usually costly and expose the patients to significant radiation.”
24. Precision Medicine for Tailored Treatment Plans
Precision medicine encompasses patients’ genetics, lifestyle, and environmental data to ensure the accuracy of personal diagnostics and treatment efficiency. The one-size-fits-all approach is based on the parameters of an average patient and overlooks a wide range of individual variables.
Cutting-edge informatics technologies and facilities are needed to effectively capture and analyze patients’ real-life data and generate accurate diagnoses and medical prescriptions. In 2023, innovative projects are expected to emerge in this niche, growing its worth to $5 billion and bringing the healthcare industry closer to the universal adoption of precision medicine.
Emerging precision informatics technologies will be secure, and interoperable, and service providers, payers, pharmaceutical firms, and other interested parties. They will exercise various diagnostic patterns to cater to the needs of different organizations and their clients.
A few that made our list:
- Synlogic. Listed Company. Founded 2014.
- AUM Biosciences. Private Company. Founded 2018.
- PierianDx. Private Company. Founded 2014.
- Kinnate Biopharma. Private Company.
- Inflammatix, Inc. Private Company.
- Owkin. Private Company.
- Atomwise. Private Company.
- Sarepta Therapeutics, Inc. Listed Company.
25. 3D Printing for Prosthetics and Surgical Guides
3D-printable prosthetics are changing the face of medicine, as engineers and physicians can develop prosthetics that are fully customized to the wearer. Consumer 3D printing is leading to an even bigger revolution: “DIY” assistive devices that can be printed by virtually anyone, anywhere.
In healthcare, 3D printing is being used to create prosthetics and surgical guides, which can help to improve patient outcomes and reduce healthcare costs in several ways:
- Customization: 3D printing allows for the creation of prosthetics and surgical guides that are customized to the specific needs of each patient. This can improve the fit and function of the device, and increase patient satisfaction.
- Speed: 3D printing can be used to create prosthetics and surgical guides in a relatively short amount of time, which can reduce wait times for patients.
- Cost-effectiveness: 3D printing can be used to create prosthetics and surgical guides at a lower cost than traditional manufacturing methods, which can help to reduce healthcare costs.
- Hero Arm is a project developed by Open Bionics, which aims to turn disabilities into superpowers with 3D-printed bionic arms for children and adults. Using Selective Laser Sintering 3D printing, with Nylon PA12, they develop prosthetics covers inspired by superheroes such as Iron Man, or fictional universes such as Star-Wars or Frozen.
- Unyq is a pioneering prosthetics company that began making leg covers for prosthetics. Their stated goal was to have prosthetics become more normalized and prove that they can show personality and uniqueness. Using 3D printing and photogrammetry to create custom prosthetic covers, Unyq has recently started producing 3D printed prosthetic leg sockets. These lightweight and aesthetically appealing sockets also contain sensors that record the health data of the wearer. As a major milestone, they’ve been approved in line with ISO standards.
What did we miss?
If we missed something let us know, we would be happy to add it to this article or others in the future.
What will the future hold? Time will tell, let’s hope in the next decade we have higher adoption and better services for patients who need it most.
Share this article and save a life!
Author:

Jonathan is a seasoned executive with a proven track record in founding and scaling digital health and technology companies. He co-founded Oatmeal Health, a tech-enabled Cancer Screening as a Service for Underrepresented patients of FQHCs and health plans, starting with lung cancer. With a strong background in engineering, partnerships, and product development, Jonathan is recognized as a leader in the industry.
Govette has dedicated his professional life to enhancing the well-being of marginalized populations. To achieve this, he has established frameworks for initiatives aimed at promoting health equity among underprivileged communities.
REVOLUTIONIZING CANCER CARE
A Step-by-Step FQHC Guide to Lung Cancer Screening
The 7-page (Free) checklist to create and launch a lung cancer screening program can save your patients’ lives – proven to increase lung cancer screening rates above the ~5 percent national average.
– WHERE SHOULD I SEND YOUR FREE GUIDE? –