Share this article and save a life!
The classic battle between time and the best interest of the patient is real in primary care.
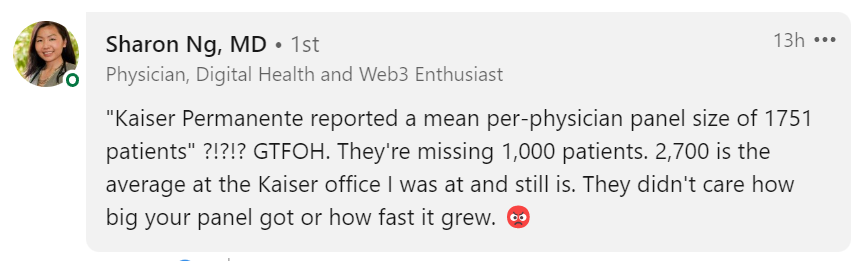
The average primary care doctor has between 1200 to 1900 patients, with Kaiser Permanente reporting a mean per-physical panel size of 1751. This most likely is not accurate nowadays, with some reports saying 2500 to 4000 is the new norm, as stated brilliantly by a LinkedIn comment by Sharon Ng M.D.
I asked my followers to share their thoughts on how they can make the healthcare system better, and they posted some great comments on this Linkedin Thread – 70 comments and counting.
What Does This Mean?
Primary care physicians often have limited time to provide comprehensive care to patients, with a focus on addressing immediate concerns rather than preventative measures.
With basic math you can see the numbers do not add up, 24 hours in a day, proper care takes 26.7 hours. And unfortunately, we are not robots that can work non-stop or manipulate time with the Infinity Gauntlet or have special powers like Dr. Strange to make up the difference.
PCPs were estimated to require 26.7 h/day, comprising
- 14.1 h/day for preventive care
- 7.2 h/day for chronic disease care
- 2.2 h/day for acute care
- 3.2 h/day for documentation and inbox management
There is this sort of disconnect between the care we’ve been trained to give and the constraints of a clinic workday,” said Justin Porter, MD, Assistant Professor of Medicine at the University of Chicago and lead author of the paper. “We have an ever-increasing set of guidelines, but clinic slots have not increased proportionately.
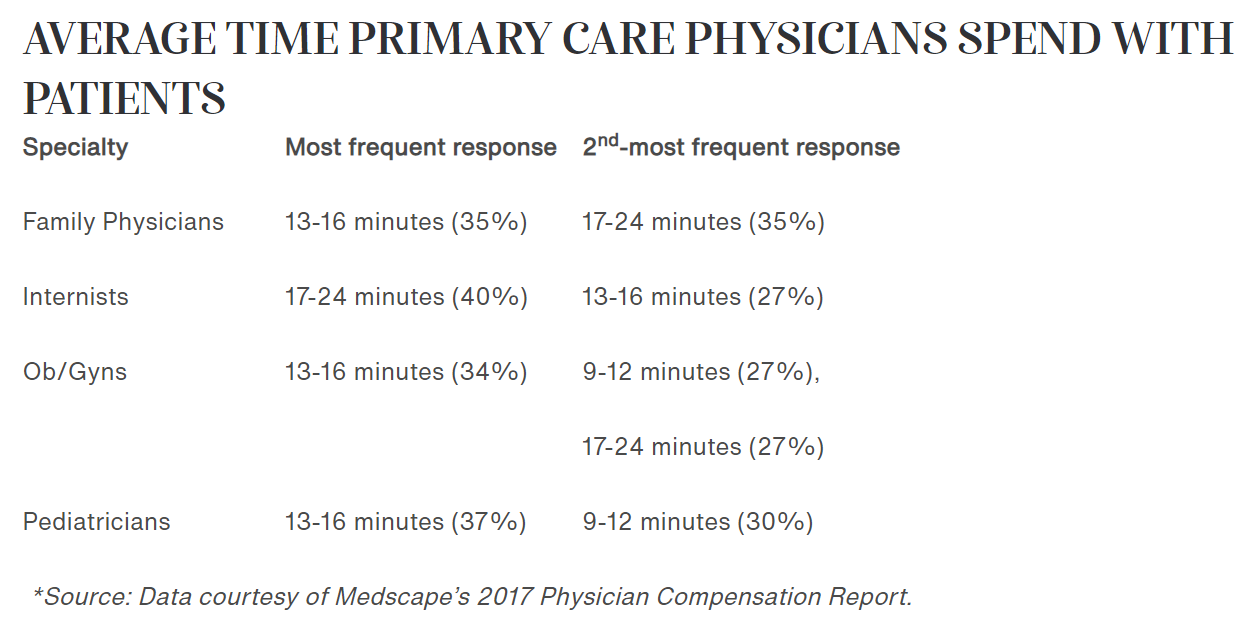
Due to the time constraints of short patient visits, often lasting only 13 to 16 minutes, primary care physicians have limited opportunities to gather information and provide education about preventative screening options, including those that may be covered by Medicare or Medicaid, such as lung cancer screening
To Many Chronic Disease Screenings to Manage
Chronic diseases are a leading cause of morbidity and mortality worldwide, and preventative screenings are the most effective way to reduce the risk of developing a chronic disease. However, many individuals do not take advantage of preventative screening services for chronic diseases, especially in rural areas.
Another study from Duke in 2005 calculated that doctors would need an additional 10.6 hours per workday to manage the top 10 chronic diseases among their patients.
And it has real consequences for the delivery of health care; the researchers said that time pressure helps explain why improvements in outcomes have not kept pace with advances made in the field, the study said.
If you do surveys with patients about what frustrates them about their medical care, you’ll frequently hear, ‘My doctor doesn’t spend time with me’ or ‘My doctor doesn’t follow up,’” said Porter in the UChicago article. “I think a lot of times this is interpreted as a lack of empathy or a lack of willingness to care for a patient. But the reality—for the majority of doctors—is simply a lack of time.
Why is this?
The bottom line is the education of the physician, time, and patient access. All things can be fixed if given the proper allocation of resources and expertise.
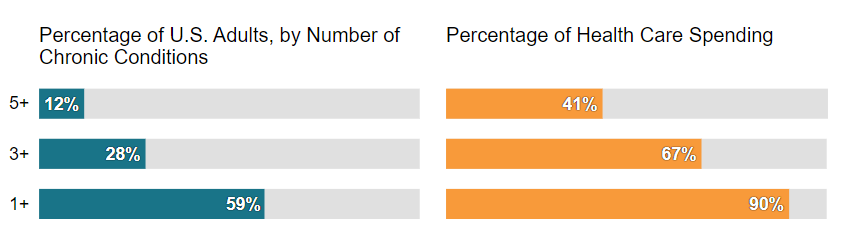
With 59% of all Americans (194 million) suffering from at least one chronic disease, and almost one in three adults having three or more chronic conditions doctors are tasked with doing the impossible, and that is why we are working to solve this issue at Oatmeal Health by partnering with FQHCs, primary care, health plans, and self-insured employers to minimize risk to patient lives and cost of care for risk-bearers.
The authors suggested “team-based care,” where nurses, physician assistants, counselors, and others help to deliver recommended care, as one solution to the problem of overworked, burned-out primary care docs.
Using team-based care, they estimated that the amount of primary care physician time could decrease to 9.3 hours per day.
About Oatmeal Health:
If you manage patients or a member population for a health plan, union, or employer, please reach out and discuss what a partnership would entail so that our team-based approach can help save lives and reduce the risk for your organization.
Share this article and save a life!
Author:

Jonathan Govette is a seasoned healthcare and technology executive with more than two decades of experience building, scaling, and advising digital health companies. He is the Co-Founder and CEO of Oatmeal Health, an AI-driven Lung Cancer Screening and Diagnostics company focused on expanding access to early detection for underrepresented populations, particularly patients served by Federally Qualified Health Centers and value-based health plans.
With a background in engineering, product development, and strategic partnerships, Jonathan has founded and led multiple health technology ventures across clinical care delivery, regulated medical software, and AI-enabled diagnostics. His work sits at the intersection of medicine, technology, and health equity, with a consistent focus on translating complex clinical problems into scalable, real-world solutions.
Jonathan has spent much of his professional life dedicated to improving outcomes for marginalized and underserved communities. He has designed and implemented frameworks that align clinical quality, reimbursement, and technology to sustainably advance health equity at scale. This mission is deeply personal and informs his leadership philosophy and long-term vision for healthcare transformation.
In addition to his operating experience, Jonathan is an author and long-time writer in the healthcare domain, with over 20 years of published work covering digital health, medical innovation, and healthcare systems. He is a frequent mentor to early-stage founders and regularly advises startups on product strategy, partnerships, and go-to-market execution in regulated healthcare environments.
Before entering industry full-time, Jonathan nearly pursued a career in medicine with an early path toward cardiothoracic surgery, an experience that continues to shape his clinical perspective and respect for frontline care delivery.
CEO | Oatmeal Health | AI Lung Cancer Startup | Engineer | Writer | Almost Became a Doctor (Cardiac Thoracic Surgeon) | 3x Health Tech Founder | Startup Mentor | Follow to share what I’ve learned along the way.