Share this article and save a life!
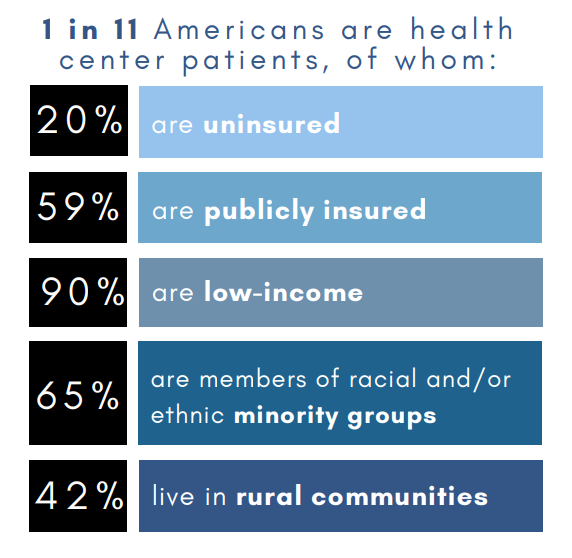
Federally Qualified Healthcare Centers (FQHCs) play a crucial role in the healthcare delivery system of the United States. According to NACHC, they serve around 30 million people, or 1 in 11 Americans, through their 1,400 centers, nearly 16,000 healthcare service sites, and 126 additional look-alike centers. Despite their importance, there is limited information available on these centers, their leaders, and the trends affecting them.
Recent interviews of FQHC CEOs by Oatmeal Health have highlighted some of the unique challenges faced by these organizations in terms of leadership, competition, and financial sustainability. The interviews found that community health centers must adopt a business mindset in order to stay open and continue serving their communities.
To help FQHCs sustain their organizations and thrive in the future, here are seven tips based on interview findings:
1. Actively pursue patient acquisition and retention
Patient acquisition and retention are critical for the success of FQHCs. The recent expansion of Medicaid has led to increased competition from provider organizations that traditionally have not focused on this segment of the market.
According to a study by the Kaiser Family Foundation, the number of individuals enrolled in Medicaid and the Children’s Health Insurance Program (CHIP) increased by 16.7 million between 2013 and 2018. This increase in Medicaid enrollment has made it more important than ever for FQHCs to actively pursue patient acquisition and retention. To stay competitive, FQHCs should assess their current marketing activities and consider conducting a comprehensive marketing audit. This will help them identify areas for improvement and develop effective patient acquisition and retention programs that are grounded in strategy, driven by return on investment (ROI), and governed by a formal marketing plan.
Ideas to improve:
- Utilize data and analytics to track and measure the effectiveness of patient acquisition and retention efforts. This will help FQHCs identify which strategies are working and which ones need to be adjusted.
- Consider implementing a customer relationship management (CRM) system to manage and track patient interactions, appointments, and follow-up care.
- Develop targeted marketing campaigns to reach specific patient populations, such as uninsured or underinsured individuals, in the community.
- Offer incentives for patients to refer friends and family to the FQHC, such as discounts on future visits or waived copays.
2. Have an appetite to compete
FQHCs should be aware of who they are competing with and why. With the expansion of Medicaid, competition is no longer limited to other FQHCs in the service area. According to a report by the Advisory Board, FQHCs face competition from various sources, including retail clinics, urgent care centers, and telehealth providers. FQHCs should use this information to differentiate how they position and communicate their services in the community. This will help them stand out and attract more patients.
Ideas to improve:
- Conduct regular market research to stay up-to-date on the competitive landscape and identify new market opportunities.
- Utilize data and analytics to track and measure the effectiveness of different service offerings, such as primary care, behavioral health, or telemedicine services.
- Develop targeted marketing campaigns that highlight the unique benefits of the FQHC, such as a focus on underserved populations or a patient-centered care approach.
- 2 companies that can offer assistance are Locutus Growth, President Megan Williams, and Insight Marketing, President Jennifer Thompson
- Consider offering extended hours or evening/weekend appointments to accommodate busy schedules and attract patients who may have difficulty accessing care during regular business hours.
- Learn what other FQHCs are doing on social media with this article – 8+ tips on how to improve your outreach to patients. – From Invisible to Invaluable: How to Effectively Market to Underinsured and Uninsured FQHC Patient Populations
3. Differentiate service offerings
Integrating mental and behavioral health with primary care is a key way for FQHCs to differentiate their services from other providers. According to a survey by the National Council for Behavioral Health, nearly 60% of FQHCs integrate behavioral health and primary care services. Other types of provider organizations may not be as focused on mental health, which gives FQHCs a critical advantage in advancing population health efforts and appeals to consumers who can obtain more services at one location.
Ideas to improve:
- Implement a patient-centered care approach, which focuses on addressing the social determinants of health, to differentiate services and improve patient outcomes.
- Develop targeted service offerings to meet the specific needs of certain patient populations, such as language-specific services for non-English speaking patients.
- Consider offering telemedicine services for patients who have difficulty accessing care in person.
- Partner with other community organizations, such as schools or shelters, to provide services and resources to patients beyond the FQHC.
4. Recruit leaders with business mindsets
To operate with a business mindset, FQHCs need leaders who have a business-minded approach. According to a survey by Sage Growth Partners, fewer than two in five CEOs (38%) believe the large majority of their current leadership (75% or more) will adequately serve the needs of their organization over the next three to five years. Leaders should consider recruiting talent from the for-profit sector to bring in new perspectives and skills. This will help them navigate the ever-changing healthcare marketplace and make strategic decisions that will benefit the organization.
Ideas to improve:
- Invest in leadership development programs to help leaders acquire the skills and knowledge necessary to operate with a business mindset.
- Consider recruiting talent from the for-profit sector to bring in new perspectives and skills.
- Develop a mentorship program to provide experienced leaders with the opportunity to share their knowledge and skills with newer leaders.
- Implement a performance management system to track and measure the performance of leaders, provide feedback, and identify areas for improvement.
5. Rethink leadership roles
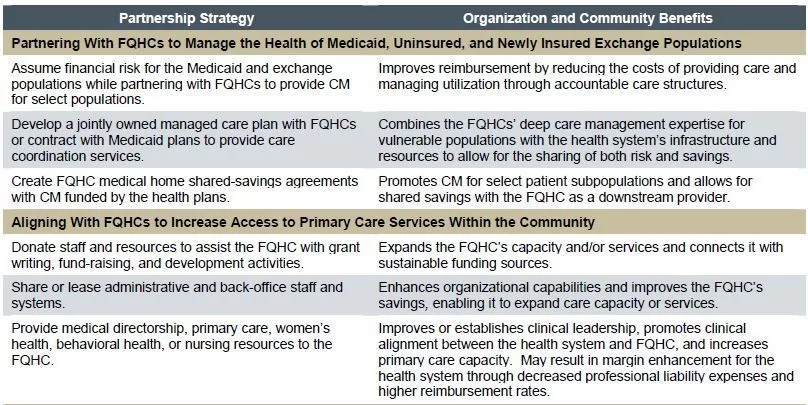
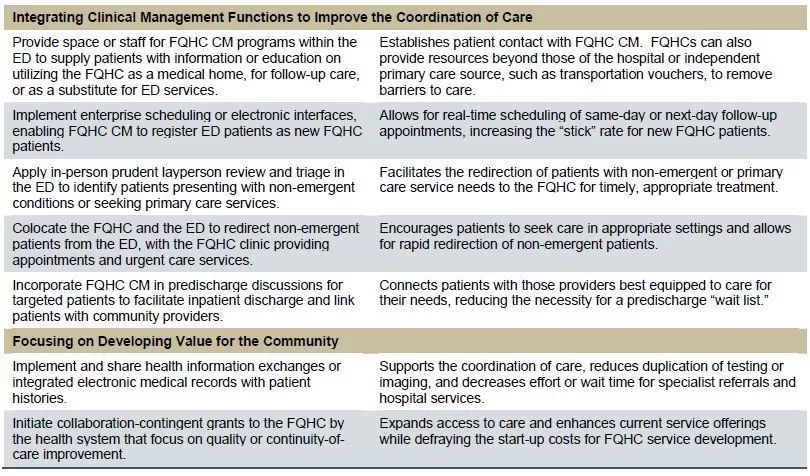
FQHCs should rethink their leadership roles to focus on enterprise population health strategies and formal partnerships with payers and hospitals. According to the National Association of Community Health Centers, FQHCs have partnerships with various types of organizations, such as hospitals, health systems, and health plans, but these partnerships tend to be informal. By formalizing these partnerships, FQHCs will be better able to align their internal and external efforts and achieve better outcomes for their patients.
Ideas to improve:
- Implement an enterprise population health management strategy to align internal and external efforts and improve patient outcomes.
- Develop a formal partnership management process to ensure that partnerships are aligned with the organization’s goals and objectives.
- Create cross-functional teams to address specific patient populations or service offerings, such as a team focused on behavioral health or a team focused on Medicaid expansion.
- Encourage leaders to participate in external professional development opportunities to stay up-to-date on the latest trends and best practices in healthcare.
6. Blur the lines between partners and competitors
FQHCs should consider deepening partnerships with other organizations, even other providers who might also be considered competitors. According to a report by Health Affairs, FQHCs and other primary care providers can increase their revenue and improve care coordination by partnering with specialists and hospitals. By doing so, they may uncover unrealized opportunities for referrals, co-location, or other partnerships that would benefit both organizations. In a previous Oatmeal Health article, physicians at FQHCs are severely overworked and do not have the time needed to offer complete preventative services such as screenings for cancer, and must partner with outside clinical services, that can offer services at a reduced or no-cost basis.
Ideas to improve:
- Implement a formal partnership management process (example of Oatmeal Health’s process) to ensure that partnerships are aligned with the organization’s goals and objectives.
- Conduct regular meetings with partners to discuss opportunities for collaboration and to identify areas for improvement.
- Create cross-functional teams to address specific patient populations or service offerings, such as a team focused on behavioral health or a team focused on Medicaid expansion.
- Encourage leaders to participate in external professional development opportunities to stay up-to-date on the latest trends and best practices in healthcare.
- Consider co-location with other healthcare providers, such as specialists or hospitals, to improve access to care for patients and increase revenue.
- Explore opportunities for shared services or joint ventures with other healthcare providers to reduce costs and improve efficiency.
- Oatmeal Health is developing a no-cost program for lung cancer screening for FQHCs. Oatmeal proactively identifies patients for cancer screening on an annual basis, utilizing a comprehensive approach that includes patient identification, shared decision-making visits, logistics coordination for CT scans, virtual nodule clinic support, and yearly follow-up, all with zero burden or resource expenditure for the patient or FQHC.
7. Embrace value-based care and population health models
Embracing value-based care and population health models is essential for the future success of FQHCs. These models focus on providing high-quality care while controlling costs and are becoming increasingly popular in the healthcare industry. By planning strategically and actively seeking out opportunities for participation in value-based care and population health initiatives, FQHCs can improve care for their patients, increase revenue, and secure their financial sustainability. Additionally, FQHCs can consider different models like Accountable Care Organizations (ACOs), Managed Care Organizations (MCOs) or Management Service Organizations (MSOs) to align with the value-based approach and help control costs and improve the population’s health.
Ideas to improve:
- Continuously monitor and measure the effectiveness of value-based care and population health initiatives, and make adjustments as needed.
- Develop a clear strategy for participating in value-based care and population health initiatives, including identifying the specific initiatives that align with the organization’s goals and objectives.
- Invest in technology and data analytics to track and measure performance in value-based care and population health initiatives.
- Provide education and training for staff on value-based care and population health models, including their role in delivering care and measuring performance.
- Seek out opportunities for collaboration with other healthcare providers, such as accountable care organizations (ACOs) or managed care organizations (MCOs) to improve care coordination and control costs.
- Consider implementing quality improvement programs to ensure that the organization is delivering high-quality care in line with the value-based care and population health models.
In summary
FQHCs play a critical role in providing healthcare to underserved communities. However, to ensure their continued success, they must adopt a business mindset and implement strategies that prioritize patient acquisition and retention, competition, service differentiation, and leadership. They should also plan strategically for value-based care and population health, and explore opportunities for partnerships and revenue gains.
Did I miss something?
If you have additions to each of the points listed above, please let us know in the comments and I will add them for others to use and share.
Share this article and save a life!
Author:

Jonathan Govette is a seasoned healthcare and technology executive with more than two decades of experience building, scaling, and advising digital health companies. He is the Co-Founder and CEO of Oatmeal Health, an AI-driven Lung Cancer Screening and Diagnostics company focused on expanding access to early detection for underrepresented populations, particularly patients served by Federally Qualified Health Centers and value-based health plans.
With a background in engineering, product development, and strategic partnerships, Jonathan has founded and led multiple health technology ventures across clinical care delivery, regulated medical software, and AI-enabled diagnostics. His work sits at the intersection of medicine, technology, and health equity, with a consistent focus on translating complex clinical problems into scalable, real-world solutions.
Jonathan has spent much of his professional life dedicated to improving outcomes for marginalized and underserved communities. He has designed and implemented frameworks that align clinical quality, reimbursement, and technology to sustainably advance health equity at scale. This mission is deeply personal and informs his leadership philosophy and long-term vision for healthcare transformation.
In addition to his operating experience, Jonathan is an author and long-time writer in the healthcare domain, with over 20 years of published work covering digital health, medical innovation, and healthcare systems. He is a frequent mentor to early-stage founders and regularly advises startups on product strategy, partnerships, and go-to-market execution in regulated healthcare environments.
Before entering industry full-time, Jonathan nearly pursued a career in medicine with an early path toward cardiothoracic surgery, an experience that continues to shape his clinical perspective and respect for frontline care delivery.
CEO | Oatmeal Health | AI Lung Cancer Startup | Engineer | Writer | Almost Became a Doctor (Cardiac Thoracic Surgeon) | 3x Health Tech Founder | Startup Mentor | Follow to share what I’ve learned along the way.