Share this article and save a life!
I decided that after interviewing hundreds of health systems and health professionals over the last decade I needed to say something again about the “health” of our healthcare system. While it is not my intent in publishing this article to call out specific companies in this article, I will provide a few examples of why some things are not doing so well.
One of my earliest articles about this topic was in 2013 when I wrote “11 reasons why our healthcare system is so messed up“, detailing some pretty damning statistics that have not gotten better in the last 10 years.
There is a multitude of reasons why the system is broken and I will go over a few here and would love to hear your thoughts in the comments as well.
A quick summary is that most FQHCs/health systems are not properly set up, trained, or qualified to manage cancer screenings and patients end up paying the price. And the price is usually time or their lives.
The current statistics are damning
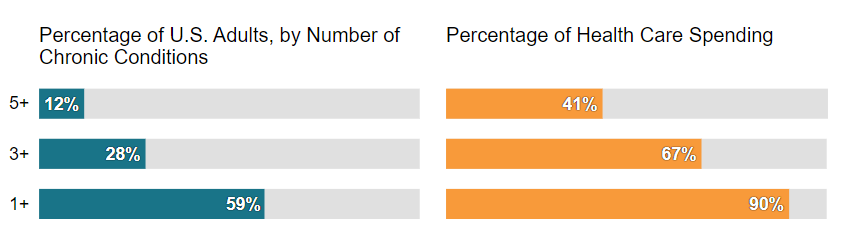
59% of all Americans (194 million) suffer from at least one chronic disease, and almost one in three adults has three or more chronic conditions. Unfortunately, the problem will only get worse with time as detailed in one of our past articles “$3.7 Trillion Reasons to Centralize Chronic Disease Management”
Story Time: FQHC in Michigan
I want to tell you a story about an FQHC in Michigan that is struggling in a few areas.
- Historical patient panel size of 25,000 patients, but is only servicing 2K to 4K patients per year.
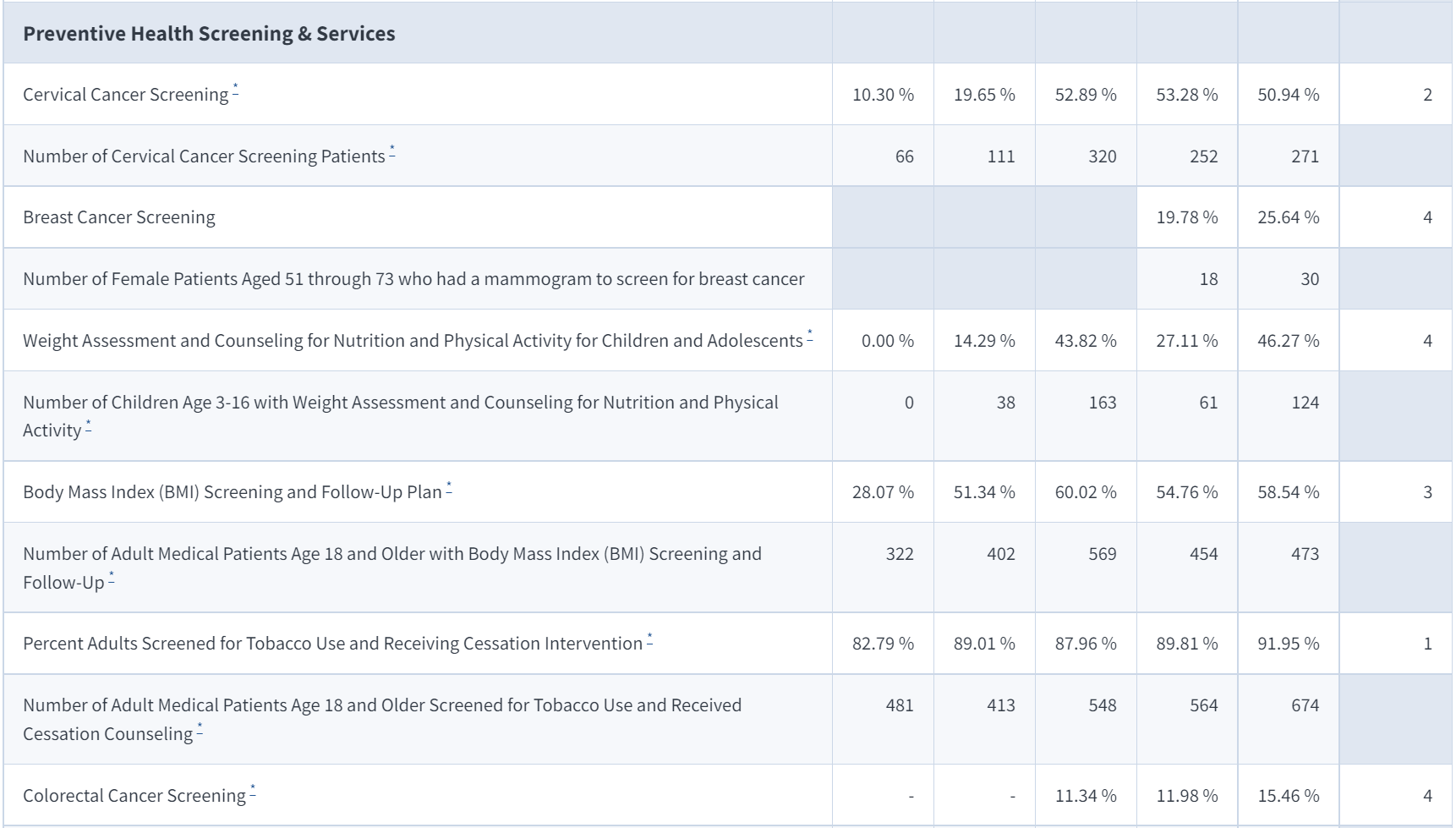
- Preventative Screenings: Lung Cancer 1%, Cervical Cancer 51%, Breast Cancer 25%, Colorectal Cancer 15%
Let’s start by saying that the staff at this unnamed FQHC is great, but they are understaffed, over budget, and their staff is overworked. They do not have the time, headcount, experience, technology, or budget to properly manage their screenings and unfortunately, patients are dying because of it.
Another very apparent challenge is they are struggling to reach their patients, which is evident by the fact that their historical patient panel size is much greater than their average patient panel this year. They are relying on antiquated tools and strategies to outreach with patients that do not work.
And unfortunately, I have looked into statistics for hundreds of FQHCs around the country and their statistics are not any better. FQHCS is tasked with managing 20 to 25 measures related to reimbursement and if done poorly CMS may assess penalties after 3 years or more of bad performance.
There is just no way for FQHCs to properly manage all these guidelines effectively and this is why a different care model is needed. One where the PCP is not required to remember or manage everything, as this is not possible based on how much time is available in a 24-hour workday.
To detail this time challenge, I recently wrote an article titled, The Battle Between Primary Care and Time: the Doctors are Losing, which describes how a standard practice would need to work 26.7 hours a day just to properly manage their patients, which is impossible.
Time: There is not enough of it
As discussed, time and unstandardized means of cancer screenings are killing patients by forgoing critical screenings until symptoms show themselves and unfortunately by then it is often too late. Is this malpractice? Is it ignorance?, is it a lack of time?, or is it the cost of doing business in America’s healthcare system?
We can fix these problems if we can agree that a primary care doctor is not superman or superwoman and that they must ask for help from partners that can do specific jobs better or have a bigger budget to assist. Just like the phrase, “It takes a village” when caring for a newborn in other countries, it takes a community to help our patients, and health systems need to start understanding this or the problem will only get worse.
FAQs about the Cost of Chronic Disease
The below statistics are just for lung cancer, but other cancers are just as problematic.
- Lung cancer is a serious national problem, it takes more lives annually in the U.S. than the next three deadliest cancers combined, breast, prostate, and pancreatic
- 1 in 17 Americans will be diagnosed with lung cancer in their lifetime.
- 13.9M underserved Americans miss their no-cost lung screening
- <5% of eligible people are screened every year for lung cancer vs 70% for breast cancer.
- Additional statistics about lung cancer
So how does an FQHC address these challenges?
One word – Partnership
Our team at Oatmeal Health addresses the most critical issue, getting the patient to come in for their appointment. While other steps are very important, all 5 steps are needed together for lung cancer screenings to be effective, and this is why less than 5 percent of the country gets screened today.
The problem is only growing, every day I hear from friends, family, and co-workers that someone in their family has cancer, had cancer, or just died of cancer. This should not be the case, but our reality is that physicians of said health systems that we have talked to just are not equipped to manage this issue and patients are dying, 7 out of 10 deaths are chronic disease-related, and many could have been prevented.
Why should an FQHC partner with Oatmeal Health?
We will toot our horn a little bit here and say, Oatmeal Health wants to partner with your FQHC to help alleviate all these challenges and offer ways to improve missed revenue opportunities without having you do any additional work. We want to take the stress off your plate, no logins, no software, and we want to ensure that your patients receive the care they need while improving your HEDIS scores at the same time.
We are starting with lung cancer today, and over time assisting with other image-based chronic diseases with our virtual nodule clinic.
How are we different from a normal radiology practice?
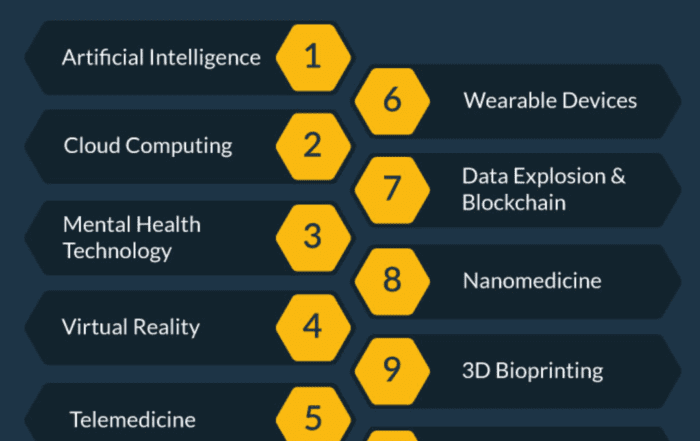
- We do all the heavy lifting, by identifying hard-to-find patients using machine learning and AI to determine who is eligible for lung cancer screening per CMS guidelines by scrubbing EHR, claims data, and UDS data.
- Once we determine who is eligible, we conduct high-touch patient outreach activities via calls, emails, texts, mail, and community outreach events to ensure patients attend their shared decision-making visit with an Oatmeal Health practitioner.
- Once the patient is identified, we immediately schedule an appointment at a local CT scanner and even arrange transportation if needed.
- We use Artificial Intelligence to read the scan and ensure the correct reading of the scan and verify with our radiology team that is credentialed in all 50 states.
- And most critically, we have advanced nudging tools to ensure the patient comes back for their 3, 6, or 12-month re-screening appointment. Radiologists are saddened that most patients never come back for future screenings, and without additional data points, we can not properly track cancer’s progress or offer treatment opportunities. This is very evident in lung cancer survivability statistics: If found early in Stage 1, lung cancer survivability is 70 – 92% versus if found late in Stage 4: 3 – 7%.
Want to learn more about Oatmeal Health?
Contact Ty Vachon M.D. to schedule a Zoom Meeting.
Start a Conversation
Have other ideas for our team to discuss, or a comment about the article? Leave a message below, we would love to hear from you in the comment section.
Share this article and save a life!
Author:

Jonathan is a seasoned executive with a proven track record in founding and scaling digital health and technology companies. He co-founded Oatmeal Health, a tech-enabled Cancer Screening as a Service for Underrepresented patients of FQHCs and health plans, starting with lung cancer. With a strong background in engineering, partnerships, and product development, Jonathan is recognized as a leader in the industry.
Govette has dedicated his professional life to enhancing the well-being of marginalized populations. To achieve this, he has established frameworks for initiatives aimed at promoting health equity among underprivileged communities.
REVOLUTIONIZING CANCER CARE
A Step-by-Step FQHC Guide to Lung Cancer Screening
The 7-page (Free) checklist to create and launch a lung cancer screening program can save your patients’ lives – proven to increase lung cancer screening rates above the ~5 percent national average.
– WHERE SHOULD I SEND YOUR FREE GUIDE? –