Share this article and save a life!
Doctors are upset!
Doctors across the country, especially those in primary care, have been up in arms about Medicare’s proposed cuts in reimbursement that are scheduled to go into effect on January 1. They are concerned — rightfully so — that these cuts will be ruinous to their practices and compromise the care they can provide to their patients.
As an emergency physician, I worry about the cuts for a different reason: emergency departments might soon be filled with more and more people who can’t access primary care.
In a recent commentary in the Washington Post, Shirlene Obuobi, a physician in Chicago, wrote about why patients no longer feel cared for by their physicians. Among other things, she described how Medicare and private insurers “reward procedures, imaging, tests and other diagnostics that generate revenue and have high reimbursement rates.”
Decreasing Payments
Falling payments to primary care doctors and generalists have forced them to increase the number of patients they see in a day, sometimes having to schedule patients every 10 minutes to justify staying open. The inevitable burnout caused by such pressures will likely drive some away from primary care, making that kind of essential care even harder to come by.
I see the consequences of this system nearly every time I work in the emergency department: the patient with headaches who have had to wait six months for a neurology appointment, the uninsured patient with newly diagnosed diabetes, or even the patient who delayed a routine mammogram and now has cancer.
Can we ever fix our ways?
The U.S. healthcare system is broken and Obuobi is right to call attention to it. But as bad as things are now, they’re going to get worse if the proposed Medicare reimbursement cuts go into effect, because even more people will find themselves unable to access primary care.
As an emergency medicine doctor, I’m trained to take care of people with heart attacks, strokes, gunshot wounds, appendicitis, broken limbs, and other time-sensitive emergencies that need prompt recognition and treatment. Yet I find myself increasingly having to address problems that would better be served by a primary care physician, things like routine management of diabetes and high blood pressure.
I like to think I’m a good doctor, but I’m not the one you want adjusting your blood pressure medicine or instructing you how to dose your insulin at home, especially not after you’ve waited six hours while I was treating people with more acute and life-threatening issues. I can’t bring you back for an appointment in two weeks to see how things are going, and I can’t be available by phone if you’re not getting better. I can’t follow your progress over time and make the adjustments that keep you healthy. It’s not what I’m trained to do, and any attempt I would make would fall woefully short of what a primary care physician can do.
It’s a shame that primary care physicians are so undervalued by the U.S. healthcare system’s reimbursement structure because the work they do is so important. More than any other physicians, they are tasked with keeping us healthy. I focus on treating decompensated disease; primary care doctors spend a lot of their time working to ensure their patients never get the disease in the first place and, if they do, it is well controlled. In addition to being important for patients, this work is also incredibly cost-effective. Ensuring that a patient with diabetes is controlling their blood sugar is far less expensive than having that patient be rushed to an emergency department in a diabetic coma.
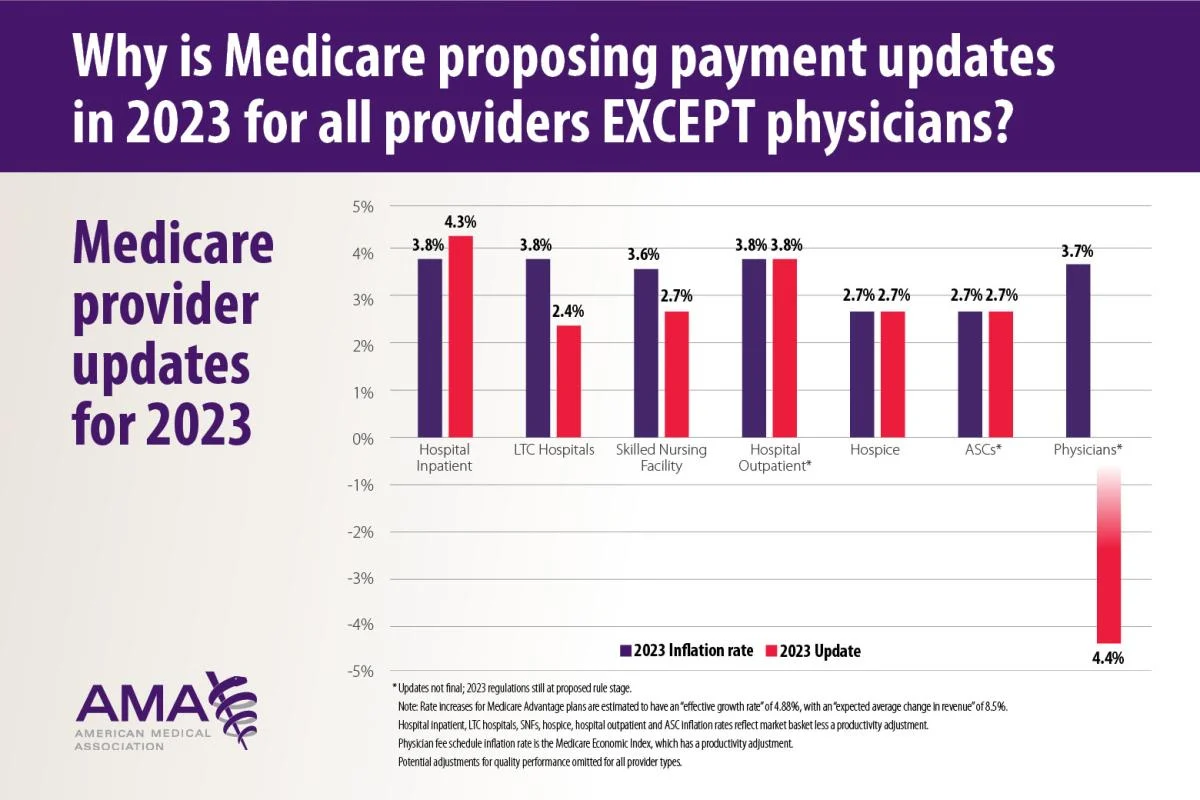
Large Medicare cuts ahead in 2023
I realize that physicians complaining about pay might not generate much sympathy from the public. But please hear me out. Many primary care physicians are in private practice, meaning they’re responsible for their own overhead. Medicare physician reimbursements are set to be cut by approximately 4% on January 1. When factored in with other projected Medicare cuts, the total cuts physicians can expect to see are closer to 8.5%. And that’s not even accounting for inflation. If reimbursements fall that dramatically, these physicians may have no choice but to stop accepting Medicare patients in order to keep their lights on. And given that most insurance companies set their reimbursement rates based on Medicare, it’s reasonable to expect that reimbursement will fall across the board, meaning that primary care doctors may be forced to accept only patients who can pay out-of-pocket.
The downstream effects of Medicare’s cuts would be devastating. People who are shut out of primary care will increasingly turn to emergency departments to meet their needs, needs these departments and their practitioners were never designed to meet. This January and beyond, in the middle of Covid-19 and flu season and the rise in RSV infections, the last thing hospitals need is more people crowding emergency departments. Yet that is exactly what will happen if the reimbursement cuts go into effect.
There is still time to act. Congress has the power to avert these pay cuts and there is currently a bill in the U.S. House of Representatives, the Supporting Medicare Providers Act of 2022 (H.R. 8800), aimed at doing just that. Yet the clock is ticking and, with under a month before the new year, I am rapidly losing hope that these cuts can be avoided.
Even if Americans don’t like to admit it, health care is a business and businesses need to be adequately paid so they can continue to offer their services. Ringing in the new year by slashing Medicare payments will hit primary care physicians the hardest, but it will be disastrous for the entire healthcare system. My colleagues and I in emergency departments across the country will be forced to try and fill the void, and we will do our absolute best to do that. But people would be much better served by readily available primary care, a business that should be rewarded for the important work it does to keep people healthy and out of emergency departments and hospitals.
Author: Greg Jasani is an emergency physician who works in Baltimore, thanks to statnews.com for first featuring this amazing content.
Share this article and save a life!
Author:
Dr Greg Jasani, MD is an emergency medicine physician who lives and works in Maryland. He obtained his MD from George Washington University before completing his residency at the University of Maryland Medical Center. He has worked in academic, private and federal hospitals throughout his career. His writing has been featured in the LA Times, Baltimore Sun, STATNews, MedPage Today, and KevinMD. He is committed to finding new and innovate solutions to improve access to healthcare in this country.