Share this article and save a life!
According to a new survey, Federally Qualified Health Centers (FQHCs) are facing a growing crisis as they struggle to recruit and retain staff while serving an ever-expanding patient population. FQHCs play a critical role in the American healthcare landscape, providing essential health services to underserved populations. But as the demand for their services grows, they are grappling with significant staffing shortages that threaten their ability to meet patient needs.
What’s the Problem?
FQHCs are tasked with helping hard-to-reach patients while at the same time managing hard-to-keep healthcare professionals due to many of the following issues.
- In 2021, NACHC reported that 95% of health centers were experiencing at least one clinical vacancy.
- The most difficult clinical positions to fill are family physicians, internists, psychiatrists, and licensed clinical social workers.
- The top reasons for staff turnover are low pay, long hours, and the stress of working in a high-need environment.
- The staffing challenges facing health centers are a major threat to their ability to provide care to their patients.
- 48% of all community health centers report a shortage of medical assistants;
- 41% report nursing shortages;
- 38% report a shortage of licensed clinical social workers; and
- 37% report shortages of dentists.
- Nearly 40% are unable to fill open positions for more than six months.
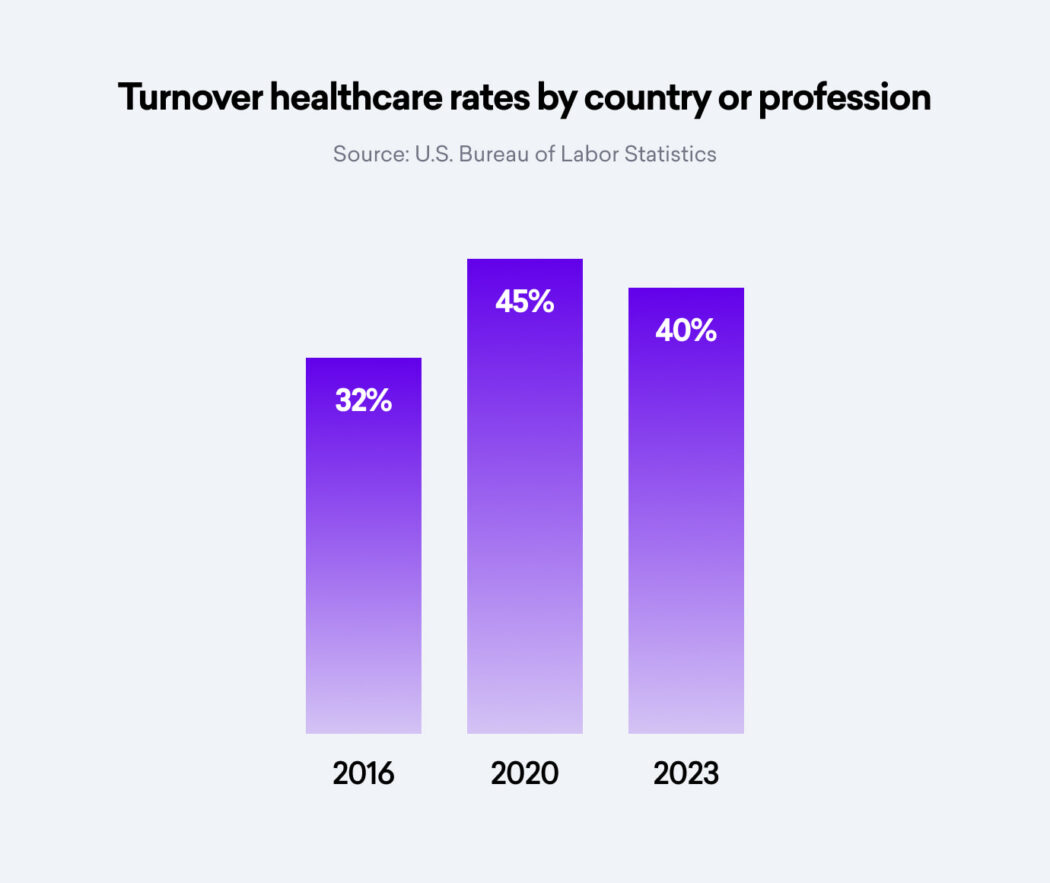
- The average turnover rate for health center staff is 32%.
The survey findings reflect the harsh reality that FQHCs are facing in their bid to serve the nation’s underserved communities. Increasing patient load, coupled with difficulties in attracting and retaining staff, is causing a worrying strain on these institutions.
Causes of the Problem
- A variety of factors contribute to this staffing challenge. Firstly, the pay scales at FQHCs are generally lower compared to private practice or larger hospital systems. This makes it difficult for FQHCs to attract and retain quality staff.
- Secondly, the rural or inner-city locations of many FQHCs often pose additional challenges. Many healthcare professionals are reluctant to relocate to these areas due to the perceived lack of amenities and opportunities.
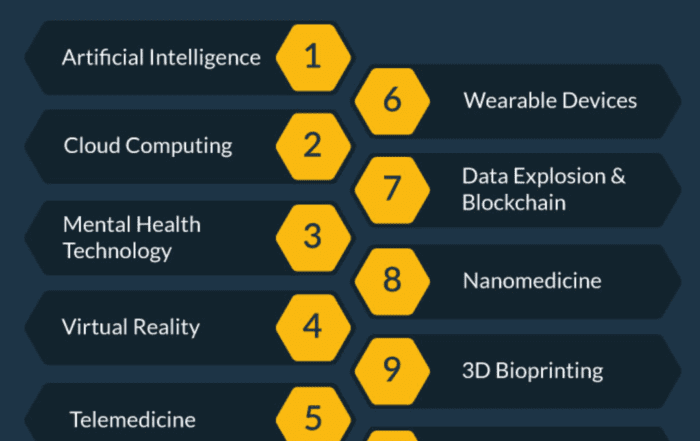
- Competition from digital health and tech-enabled services that can pay higher salaries and benefits can attract talent away from FQHCs.
- Lastly, the pandemic has further exacerbated the situation. The increased healthcare demand and stress levels caused by COVID-19 have led to burnout, forcing many healthcare professionals to leave the industry or seek less stressful environments.
Solutions and Steps to Address the Problem
Despite the challenges, the situation is not hopeless. Several strategies can be implemented to attract and retain staff at FQHCs:
1. Competitive Compensation: FQHCs need to review and adjust their pay scales to be more competitive. This will not only attract new talent but also encourage existing staff to stay.
The issue of competitive compensation is a critical one for Federally Qualified Health Centers (FQHCs). Often, these centers are unable to match the salaries offered by private practices or larger healthcare systems. This wage gap can make it challenging to attract and retain high-quality healthcare professionals, which are crucial for the effective delivery of services.
Competitive compensation is not only about the base salary. It encompasses a holistic approach to remuneration, considering factors such as benefits packages, bonuses, allowances, and other non-monetary incentives. A comprehensive, competitive compensation package can help FQHCs to stand out as attractive employers in the healthcare sector.
- Salary Review and Adjustment:
The first step FQHCs can take is to conduct regular salary reviews. This involves benchmarking salaries against those in comparable positions in the private sector and other healthcare systems. While FQHCs may struggle to match these salaries due to funding constraints, understanding the market rate can help these centers determine how much they need to adjust their pay scales to be more competitive.
- Benefits Packages:
In addition to salaries, FQHCs should also consider the benefits they offer. These could include health insurance, retirement plans, paid time off, and other perks. A robust benefits package can significantly enhance the total compensation package, making the job offer more attractive to potential employees.
- Non-Monetary Incentives:
While salaries and benefits are important, FQHCs can also attract and retain staff through non-monetary incentives. These could include flexible working hours, opportunities for professional development, a positive work environment, and the chance to make a difference in underserved communities. FQHCs have a unique value proposition in this regard, as their work has a direct, tangible impact on community health.
- Advocacy for Increased Funding:
Of course, increasing compensation often requires additional funding. Therefore, FQHCs and organizations like the National Association of Community Health Centers (NACHC) need to continue advocating for increased state and federal funding. This could include lobbying for policy changes that increase the financial resources available to FQHCs.
By taking a comprehensive approach to competitive compensation, FQHCs can attract new talent and encourage existing staff to stay, thus addressing one of the key challenges they face in their staffing efforts.
2. Loan Forgiveness Programs: Many healthcare professionals graduate with significant student loan debt. FQHCs can partner with federal and state agencies to offer loan forgiveness programs for those willing to serve in underserved areas.
Loan forgiveness programs can serve as a powerful incentive for healthcare professionals to work in Federally Qualified Health Centers (FQHCs). These programs typically involve the reduction or elimination of student loan debt in exchange for a commitment to work in an underserved area for a certain period.
- How Loan Forgiveness Programs Work:
These programs generally work by providing financial assistance to repay educational loans. In the case of healthcare professionals, this could cover loans acquired during undergraduate or medical school. The program participants agree to serve in an FQHC or a similar setting in an underserved area for a specified number of years.
- Benefits to Healthcare Professionals:
For many healthcare professionals, particularly recent graduates, student loan debt can be a significant burden. Loan forgiveness programs can provide substantial financial relief, making positions at FQHCs more attractive despite potentially lower salaries compared to private practices or larger healthcare systems.
- Partnerships with Federal and State Agencies:
FQHCs can partner with federal and state agencies to offer these programs. For example, the National Health Service Corps (NHSC) Loan Repayment Program is a federal initiative that provides up to $50,000 towards student loans in exchange for two years of work at an NHSC-approved site, many of which are FQHCs.
States often have their own loan repayment programs as well. For instance, the California State Loan Repayment Program offers up to $50,000 in repayment assistance for healthcare providers who commit to serving in a Health Professional Shortage Area (HPSA) for at least two years.
- Advocacy for Expanded Programs:
While these programs can be effective, there is room for growth and expansion. FQHCs and organizations like the National Association of Community Health Centers (NACHC) can advocate for increased funding and expanded eligibility for these programs. This can help attract a wider range of healthcare professionals to FQHCs and similar settings.
By leveraging loan forgiveness programs, FQHCs can attract motivated healthcare professionals committed to serving underserved communities, reducing the burden of student loan debt, and increasing the overall appeal of working in these settings.
3. Enhanced Training and Development: By providing ongoing training and development opportunities, FQHCs can demonstrate their commitment to their staff’s professional growth. This can lead to increased job satisfaction and lower turnover rates.
Investment in training and development can be an effective strategy for Federally Qualified Health Centers (FQHCs) to recruit and retain staff. By offering opportunities for continuous learning and professional growth, FQHCs can make themselves more attractive to prospective and current employees.
- Continuous Learning:
Healthcare is a rapidly evolving field, and healthcare professionals need to stay updated with the latest practices, research, and technologies. FQHCs can support this by offering regular training sessions, workshops, and seminars. This could cover a range of topics, from the latest medical research to new technologies or techniques in healthcare.
- Professional Development Opportunities:
Beyond job-specific training, FQHCs can also provide broader professional development opportunities. This might include leadership training for those looking to move into managerial roles, or further education assistance for those who wish to specialize or further their qualifications.
- Mentorship Programs:
Mentorship programs can also be a valuable part of a development strategy. By pairing less experienced staff with seasoned professionals, FQHCs can facilitate knowledge transfer and foster a supportive and collaborative work environment.
- Recognition of Achievements:
Recognition of achievements and growth can also be a crucial element in a training and development strategy. This could include acknowledging the completion of training programs, the attainment of new qualifications, or exceptional performance in the workplace. Recognition not only motivates employees but also fosters a culture of continuous learning and improvement.
- Benefits to FQHCs and Staff:
By providing training and development opportunities, FQHCs can create a more competent and confident workforce. This not only enhances the quality of care provided to patients but can also lead to increased job satisfaction and employee retention. Employees who feel that their employer is invested in their professional growth are more likely to stay with the organization.
- Challenges and Funding:
Of course, these programs require resources and planning. FQHCs may need to seek additional funding or partnerships to support these initiatives. However, the potential benefits in terms of staff recruitment, retention, and patient care quality make this a worthwhile investment.
In conclusion, enhanced training and development opportunities can play a significant role in addressing the staffing challenges faced by FQHCs. It not only helps in attracting new talent but also encourages existing staff to continue their career journey within the organization.
4. Work-Life Balance Initiatives: Burnout is a significant factor driving healthcare professionals away from the industry. Implementing policies that support work-life balance, such as flexible hours, stress management programs, and mental health support, can help retain staff.
- Flexible Work Arrangements:
One key aspect of work-life balance initiatives is flexible work arrangements. This could include flexible scheduling, such as allowing employees to adjust their start and finish times, or offering part-time positions. It could also involve remote work opportunities, where applicable.
- Paid Time Off:
Another important factor is paid time off. This includes not only vacation days but also sick leave and personal days. Ensuring that employees can take time off when they need it without financial repercussions can significantly improve work-life balance.
- Wellness Programs:
Wellness programs can also contribute to work-life balance. These programs could include fitness classes, mental health resources, stress management seminars, or other health-related initiatives. Some FQHCs might also consider offering services like on-site childcare or assistance with elder care, which can ease some of the personal responsibilities that can interfere with work.
- Employee Assistance Programs:
Employee Assistance Programs (EAPs) can be another valuable resource. EAPs typically provide services like counseling, legal advice, financial planning, and more. These resources can help employees manage personal issues that might otherwise impact their work and overall well-being.
- Creating a Supportive Culture:
Beyond specific programs and policies, FQHCs should strive to create a culture that values work-life balance. This includes respecting boundaries (like not expecting employees to respond to emails outside of work hours), recognizing and rewarding hard work, and encouraging employees to take time for themselves.
- Benefits to FQHCs and Staff:
Work-life balance initiatives can lead to numerous benefits. Employees who feel that their work-life balance is respected are likely to have higher job satisfaction, better performance, and lower rates of burnout. This can lead to lower turnover rates, making it easier for FQHCs to retain staff.
5. Community Integration: FQHCs can work closely with local communities to create welcoming and inclusive environments for their staff. This can make relocating to underserved areas more attractive.
Federally Qualified Health Centers (FQHCs) serve as vital hubs of healthcare in their communities, particularly in underserved areas. Thus, integrating into these communities can be a powerful strategy for FQHCs, both in terms of providing better service to their patients and attracting and retaining staff.
- Understanding Community Needs:
By engaging with their communities, FQHCs can gain a better understanding of local needs and challenges. This can inform their services, ensuring they are effectively meeting the health needs of the community. This could involve holding community meetings, conducting surveys, or partnering with local organizations.
- Fostering Relationships with Local Institutions:
FQHCs can also foster relationships with local institutions, such as schools, universities, businesses, and other organizations. These partnerships can lead to collaborative initiatives, such as health education programs, community health events, or internship and training opportunities for local students.
- Creating Welcoming Environments:
Community integration also means creating a welcoming and inclusive environment for staff. This could involve supporting local culture and traditions or offering local language services. For staff who are relocating to work at the FQHC, assistance with finding housing, understanding local services, and integrating into the community can be beneficial.
- Benefits of Community Integration:
Community integration has many benefits. It can enhance the services provided by FQHCs, making them more responsive to community needs. It can also improve the community’s perception of the FQHC, making it a more attractive place to work.
For healthcare professionals, working in a community-integrated FQHC can provide a sense of purpose and fulfillment. It offers an opportunity to make a tangible difference in the health and well-being of the community. This can be a powerful incentive for recruitment and retention, particularly for those motivated by a desire to serve.
6. Advocacy: FQHCs can collaborate with organizations like NACHC to advocate for policy changes that support their staffing needs. This can include lobbying for increased funding or regulatory changes that make it easier to recruit and retain staff.
Advocacy plays a critical role in addressing the staffing challenges faced by Federally Qualified Health Centers (FQHCs). By actively advocating for policy changes, increased funding, and regulatory revisions, FQHCs can create a more conducive environment for attracting and retaining staff.
- Policy Changes:
FQHCs can lobby for policy changes that directly impact their staffing needs. This could involve advocating for policies that improve compensation for healthcare professionals working in underserved areas, or that expand loan forgiveness programs.
Moreover, FQHCs can advocate for policy changes that address some of the root causes of their staffing challenges. For instance, they could lobby for policies aimed at improving living conditions in underserved areas, thereby making these locations more attractive to healthcare professionals.
- Increased Funding:
Funding is a key issue for FQHCs. Advocacy efforts can focus on securing more substantial and consistent funding from local, state, and federal governments. Increased funding can enable FQHCs to offer more competitive salaries, invest in training and development, and improve their facilities and services, all of which can help attract and retain staff.
- Regulatory Revisions:
FQHCs can also advocate for regulatory changes that would facilitate recruitment and retention. For example, they might lobby for revisions to licensing requirements that make it easier for healthcare professionals from other states or countries to practice.
- Collaboration with Organizations:
FQHCs can collaborate with organizations like the National Association of Community Health Centers (NACHC) at tech-enabled services like Oatmeal Health to strengthen their advocacy efforts. These organizations have the expertise, resources, and networks to effectively lobby for policy, funding, and regulatory changes.
- Public Awareness:
In addition to direct lobbying, FQHCs can also engage in advocacy aimed at increasing public awareness and understanding of the important role they play in providing healthcare to underserved communities. This can help garner public support for their cause, adding weight to their advocacy efforts.
Share this article and save a life!
Author:

Jonathan is a seasoned executive with a proven track record in founding and scaling digital health and technology companies. He co-founded Oatmeal Health, a tech-enabled Cancer Screening as a Service for Underrepresented patients of FQHCs and health plans, starting with lung cancer. With a strong background in engineering, partnerships, and product development, Jonathan is recognized as a leader in the industry.
Govette has dedicated his professional life to enhancing the well-being of marginalized populations. To achieve this, he has established frameworks for initiatives aimed at promoting health equity among underprivileged communities.
REVOLUTIONIZING CANCER CARE
A Step-by-Step FQHC Guide to Lung Cancer Screening
The 7-page (Free) checklist to create and launch a lung cancer screening program can save your patients’ lives – proven to increase lung cancer screening rates above the ~5 percent national average.
– WHERE SHOULD I SEND YOUR FREE GUIDE? –