Share this article and save a life!
Cancer screenings save lives.
They saved my mother’s life. Her breast cancer was found on a routine mammogram. She was the anomaly; no personal or family history of breast cancer and no other risk factors. In fact, she was so sure that her mammogram would be normal that she almost delayed getting it; wanting instead to help my wife and me with our newborn. I’m so glad she didn’t. While learning that she had cancer was devastating to all of us, it was caught at a very early and treatable stage. I’m happy to say my mom has been cancer free now for over a year.
Her story, though, perfectly encapsulates why we in the medical community put so much emphasis on screenings. They work and they save lives. It’s much better to catch cancer when it’s a small lump in the breast than when it has spread to lymph nodes, bone, and brain. Currently, in the United States, it is recommended that everyone is regularly screened for breast, cervical, and colorectal cancers. Patients at high risk for lung cancer should also be regularly screened for suspicious nodules. Although not broadly recommended, prostate-specific antigen tests (PSA) can also be used as a screen for prostate cancer.
You can imagine my dismay, then, when I learned how horrible our screening success rates are. According to researchers from the University of Chicago, only 14% of all cancers diagnosed are caught on a preventative screening exam. Think about that: that means that our screening exams are not even catching 1 in every 5 cancer cases. Would you get on an airplane if you knew its maintenance crew was only finding 14% of all mechanical problems before takeoff? Of course not!
Now, admittedly, part of why this rate is so low is that there are many cancers for which no recommended screening exists. The researchers at the University of Chicago estimate that 57% of all cancers diagnosed in this country do not currently have an accepted screening method. This category is broad and includes malignancies such as leukemia, brain cancer, throat cancer, and even highly aggressive pancreatic cancer.
However, even among the screenable cancers, the success rates still leave a lot to be desired. Amazingly, despite not having widespread acceptance, prostate cancer is the most successfully screened for malignancy with 77% of all cases diagnosed on a screening exam. Breast cancer catch rates are also good with a rate of 61%. After that, though, the success rates drastically drop off. Only about half of all cervical and colorectal cancers are being caught at the screening stage. For lung cancer, the results are absolutely abysmal; only 3% of all lung cancers are being caught by routine, recommended screening exams. That is unacceptable for cancer which accounts for more deaths than breast, pancreatic and colorectal combined.
Of course, this begs the question: if routine screening exams are not diagnosing these cancers, who is? Well, part of the answer is me. As an emergency medicine physician, I have diagnosed plenty of patients with cancer. It’s not my job to diagnose cancer; my job is to look for acute diseases that require immediate treatment. Despite what you may think, cancer rarely falls into this category. While a devastating disease, it rarely presents the immediate threat to life that I am tasked with recognizing and treating.
My cancer diagnoses are not deliberate but often result from accidents.
The CT scan of the brain I get to look for a stroke shows a new mass or the chest x-ray I get to look for pneumonia shows a suspicious nodule. Worst of all, the CT scan of the abdomen I get to look for appendicitis instead shows multiple masses, showing that what was once probably a localized malignancy has now metastasized, carrying a much worse prognosis for my patient.
I’ve had to tell patients that they have cancer. It’s never a fun conversation and, quite frankly, one I should not be having. The news that you have cancer should come from someone you know and trust; someone like your primary care doctor. As an emergency medicine physician, I don’t have that relationship with my patients. I’ve often only met the person I am giving this devastating news to only an hour ago. I don’t have the same level of rapport with this patient yet I am the one tasked with delivering life-altering news. Not surprisingly, I’ve faced reactions ranging from disbelief to outright hostility. I can’t blame them; I can’t imagine how I’d react if a stranger told me I had cancer.
We need to wake up, patients are dying
The absolutely horrendous cancer screening rates should be a wake-up call to the U.S. healthcare system, a wake-up call that the status quo is unacceptable and significant changes must occur. Sadly, I don’t see that happening anytime soon. Cancer screening falls within the realm of primary care. Unfortunately, due to a multitude of reasons, primary care in this country is already inaccessible to many. Additionally, it shows no signs of improvement as targeted Medicare physician reimbursement cuts are only going to exacerbate the problem.
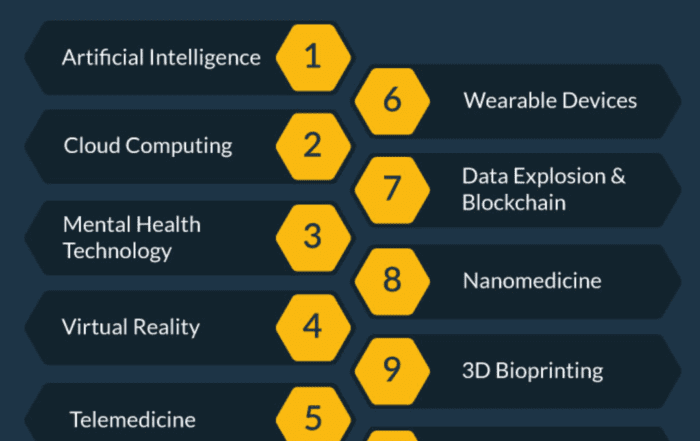
What this means, then, is that we must begin to think beyond the traditional healthcare delivery model to find impactful solutions to this problem. Telehealth, a field that has made significant strides because of the COVID pandemic, shows great promise in expanding care to those who would otherwise fall through the cracks of the U.S. healthcare system. Similarly, many healthcare startups and nonprofits are beginning to focus on preventative care. Further expansion and refinement of both of these options should be encouraged by healthcare providers and stakeholders alike.
The failure of our cancer screening system should be a call to action for all of us in healthcare. For me, this issue is personal. I’ve experienced both ends of the spectrum: the immense benefit of catching cancer early and the heartbreak when I have to tell someone whose screening failed that they have cancer. Every patient deserves the level of care my mother got and no patient should hear that they have cancer from me or my fellow emergency medicine colleagues.
I dream of a day when I never have to deliver the news of a cancer diagnosis to a patient. Getting to that goal will require new, bold thinking and drastic changes to how we deliver healthcare to our patients. Yet, I am hopeful that by embracing new modes of healthcare delivery, such as telehealth, we can catch more cancers in the early, treatable stages and save more lives.
Share this article and save a life!
Author:
Dr Greg Jasani, MD is an emergency medicine physician who lives and works in Maryland. He obtained his MD from George Washington University before completing his residency at the University of Maryland Medical Center. He has worked in academic, private and federal hospitals throughout his career. His writing has been featured in the LA Times, Baltimore Sun, STATNews, MedPage Today, and KevinMD. He is committed to finding new and innovate solutions to improve access to healthcare in this country.
REVOLUTIONIZING CANCER CARE
A Step-by-Step FQHC Guide to Lung Cancer Screening
The 7-page (Free) checklist to create and launch a lung cancer screening program can save your patients’ lives – proven to increase lung cancer screening rates above the ~5 percent national average.
– WHERE SHOULD I SEND YOUR FREE GUIDE? –