Share this article and save a life!
A sliding scale fee is a vital tool for Federally Qualified Health Centers (FQHCs) to ensure that low-income and underserved patients can access essential healthcare services. It allows FQHCs to charge fees based on a patient’s income and household size, making healthcare affordable for all patients, regardless of their financial circumstances. The following guide provides detailed steps for creating and implementing a sliding scale fee for FQHCs:
Step 1: Understand Federal Guidelines and Requirements
Before creating a sliding scale fee, FQHCs must familiarize themselves with the federal guidelines and requirements set by the Health Resources and Services Administration (HRSA). According to HRSA guidelines, FQHCs must offer a sliding fee discount program (SFDP) to eligible patients based on their income and family size, using the Federal Poverty Guidelines (FPG) as a reference.
According to HRSA guidelines, FQHCs are required to offer a sliding fee discount program (SFDP) to eligible patients. The SFDP is a critical component of FQHCs’ commitment to providing affordable healthcare services to underserved populations. To implement an SFDP, FQHCs must adhere to the following key requirements:
- Fee schedule: FQHCs must develop a fee schedule for their services that reflects the actual cost of providing care. The schedule should include both full fees and discounted fees, based on patients’ income levels and family size.
- Federal Poverty Guidelines (FPG) reference: The SFDP must use the FPG as a reference to determine the eligibility of patients for discounts. The FPG is updated annually by the U.S. Department of Health and Human Services and serves as a benchmark for assessing income levels in relation to poverty.
- Income-based discounts: FQHCs must offer discounts to patients with incomes at or below 200% of the FPG. The discounts should be structured on a sliding scale, with deeper discounts provided to patients with lower incomes.
- Nominal charges: For patients with incomes below the FPG, FQHCs may apply nominal charges for services instead of offering free care. These nominal charges should not be a barrier to accessing care and should be based on the patient’s ability to pay.
- No denial of services: FQHCs must not deny services to patients due to their inability to pay, even if they cannot afford the nominal charges. The emphasis should be on providing care to all, regardless of financial circumstances.
- Public notice: FQHCs must inform patients about the availability of the SFDP through clear and easily accessible means, such as signage, brochures, and online information.
- Regular review and updates: FQHCs should regularly review and update their SFDP to ensure compliance with the HRSA guidelines and to accommodate changes in the FPG and other relevant factors.
Step 2: Determine Fee Structure
The sliding scale fee structure typically consists of three main components:
- Full Pay: Patients with incomes above a certain percentage of the FPG (e.g., 200%) pay the full cost of services.
- Partial Discount: Patients with incomes between certain percentages of the FPG (e.g., 100-200%) pay a reduced fee based on their income level.
- Minimum Fee or Nominal Charge: Patients with incomes below a specific percentage of the FPG (e.g., 100%) pay a minimum fee or a nominal charge.
FQHCs should develop a fee structure that offers appropriate discounts based on the patient’s income level and meets the HRSA requirements.
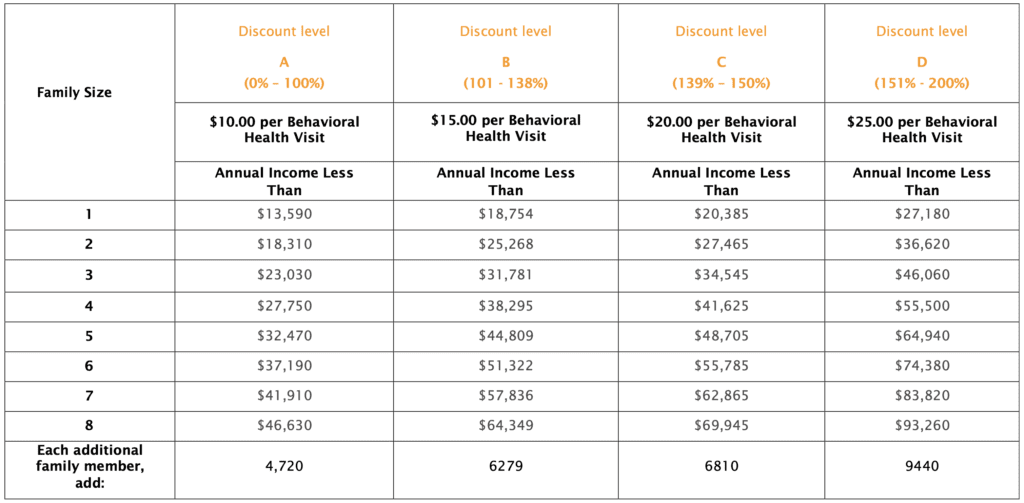
Example: Cempa Community Health
Step 3: Develop a Sliding Scale Fee Schedule
Using the determined fee structure, create a sliding scale fee schedule that outlines the discounts available to patients at each income level. The schedule should clearly indicate the income ranges and corresponding fees for each service provided by the FQHC. Ensure that the fee schedule is updated annually to reflect changes in the FPG.
Step 4: Establish Eligibility Criteria and Documentation Requirements
Develop clear eligibility criteria for patients to qualify for the SFDP, based on their income and family size. Determine the documentation requirements necessary for patients to demonstrate their eligibility, such as proof of income (e.g., pay stubs, tax returns, or benefit statements) and proof of family size (e.g., birth certificates or school enrollment forms).
Step 5: Train Staff on the Sliding Scale Fee Policy
Train all staff members, including front desk personnel, billing staff, and healthcare providers, on the sliding scale fee policy and procedures. Ensure that staff understands how to assess patients’ eligibility for the SFDP, explain the fee structure to patients, and collect fees in a compassionate and culturally sensitive manner.
Step 6: Communicate the Sliding Scale Fee Policy to Patients
Inform patients about the availability of the SFDP through various channels, such as signage in the waiting area, brochures, and the FQHC’s website. Clearly explain the eligibility criteria, documentation requirements, and application process to help patients understand and access the program.
Step 7: Monitor and Evaluate the Sliding Scale Fee Program
Regularly monitor and evaluate the effectiveness of the sliding scale fee program to ensure it meets the needs of the FQHC’s patient population and complies with HRSA guidelines. Analyze the impact of the program on patient access to care, financial sustainability, and patient satisfaction. Adjust the program as necessary based on evaluation findings and changes in the FPG or HRSA requirements.
Additional Tips for Successful Implementation:
- Develop a clear written policy: Create a written policy outlining the sliding scale fee program, including eligibility criteria, documentation requirements, fee structure, and application process. This policy will serve as a reference for staff and ensure consistent implementation across the organization.
- Offer flexible payment options: To further support patients with financial difficulties, consider offering flexible payment options such as payment plans, delayed payments, or the ability to pay in installments. This can help reduce the financial burden on patients while still generating revenue for the FQHC.
- Regularly review and update the policy: Periodically review and update the sliding scale fee policy to reflect changes in the FPG, HRSA guidelines, or the FQHC’s patient population and service offerings. This will help ensure that the program remains effective and compliant with federal requirements.
- Engage in community outreach: Promote the sliding scale fee program within the community to raise awareness and encourage eligible patients to seek care at the FQHC. Collaborate with local organizations, schools, and faith-based institutions to spread the word about the program and its benefits.
- Collect and analyze data: Collect data on the sliding scale fee program’s impact on patient access to care, financial sustainability, and patient satisfaction. Analyze this data to identify areas for improvement and inform future program adjustments.
Share this article and save a life!
Author:

Jonathan is a seasoned executive with a proven track record in founding and scaling digital health and technology companies. He co-founded Oatmeal Health, a tech-enabled Cancer Screening as a Service for Underrepresented patients of FQHCs and health plans, starting with lung cancer. With a strong background in engineering, partnerships, and product development, Jonathan is recognized as a leader in the industry.
Govette has dedicated his professional life to enhancing the well-being of marginalized populations. To achieve this, he has established frameworks for initiatives aimed at promoting health equity among underprivileged communities.
REVOLUTIONIZING CANCER CARE
A Step-by-Step FQHC Guide to Lung Cancer Screening
The 7-page (Free) checklist to create and launch a lung cancer screening program can save your patients’ lives – proven to increase lung cancer screening rates above the ~5 percent national average.
– WHERE SHOULD I SEND YOUR FREE GUIDE? –