Share this article and save a life!
Federally Qualified Health Centers (FQHCs) are community-based healthcare providers that serve low-income, underserved, and vulnerable populations.
They offer essential primary and preventive care services to individuals regardless of their ability to pay. Despite the invaluable services FQHCs provide, they often face financial challenges due to their reliance on grants and government funding.
This dependence can lead to negative consequences for patients when funding is cut, including loss of healthcare access and, in some cases, death. This article will explore the importance of diversifying funding sources for FQHCs to ensure their long-term sustainability and continued provision of vital healthcare services.
The Importance of FQHCs
FQHCs play a critical role in the healthcare system by providing accessible, high-quality care to vulnerable populations. They offer a wide range of services, including primary care, dental care, mental health services, substance abuse treatment, and health education. FQHCs often serve as the primary source of healthcare for individuals who would otherwise have limited or no access to care, such as those without insurance, low-income families, and individuals in rural or remote areas. By addressing the unique needs of these populations, FQHCs contribute significantly to reducing health disparities and promoting health equity in the United States.
The Perils of Grant Dependency
Grants from the government and other funding organizations play a significant role in supporting FQHCs, enabling them to provide vital services to the communities they serve. However, grant funding is often temporary, and when it runs out or is cut, FQHCs can experience severe financial instability. The consequences of funding cuts can be dire for patients, with many losing access to essential healthcare services. In some cases, patients with chronic conditions or life-threatening illnesses may face severe suffering or even death due to the discontinuation of care.
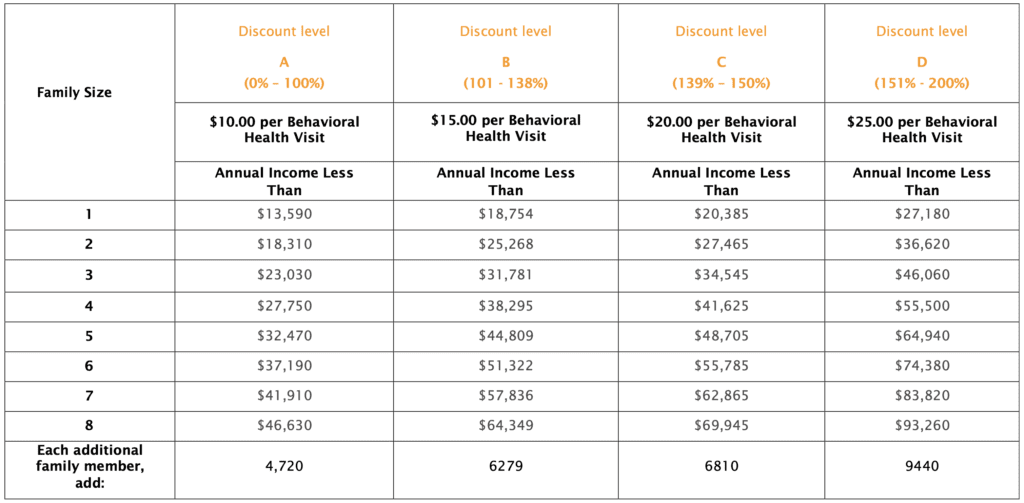
To protect anonymity: This case is representative of the many health centers across the nation that screen only a fraction of their patient population – typically 20 to 40 percent – leading to preventable deaths. Through my interviews with numerous facilities, it has become clear that most lack the necessary resources – funding, technology, or staffing – to conduct thorough screening for all patients.
Diversifying Funding Sources for FQHCs
To ensure the long-term sustainability of FQHCs and protect the health and well-being of the patients they serve, it is crucial for these organizations to diversify their funding sources. By tapping into a variety of revenue streams, FQHCs can create a more stable financial foundation, reducing their vulnerability to funding cuts and fluctuations. The followings are some ideas and tips for FQHCs to diversify their funding and enhance their financial sustainability:
1. Cultivate Strong Relationships with Local Businesses and Corporations
FQHCs can partner with local businesses and corporations to secure funding and in-kind donations, such as office supplies, medical equipment, and volunteer services. By forging these partnerships, FQHCs can tap into new funding sources while strengthening their community ties and raising awareness about their services.
FQHCs can create a list of potential business partners in their community and reach out to them with a tailored proposal highlighting the benefits of partnering with the health center. Providing clear and concise information on the impact their support will have on the community can help convince businesses to get involved.
Example: The Family Health Centers of San Diego (FHCSD) partnered with Qualcomm, a local technology company, to receive funding and support for their programs and services. This partnership not only provides FHCSD with financial resources but also strengthens its community presence and raises awareness about its services.
2. Develop a Robust Individual Donor Program
Engaging individual donors is another critical component of a diversified funding strategy. FQHCs should invest in building relationships with current and potential donors, emphasizing the impact of their services on the health and well-being of the community. Regular communication, events, and targeted fundraising campaigns can help to inspire donor loyalty and increase donations.
Start by identifying and segmenting your current and potential donor base. Develop targeted messaging and outreach strategies for each group, and plan events or campaigns that cater to their interests. Maintain regular communication with donors through newsletters and social media, keeping them informed about the impact of their contributions.
Example: Zufall Health, an FQHC in New Jersey, hosted a fundraising event called “30+1” to engage individual donors and raise funds for their services. The event offers a chance for donors to connect with the health center’s mission, hear success stories, and contribute to the cause.
3. Apply for Foundation Grants
In addition to government grants, FQHCs should pursue funding from private and corporate foundations. These grants can offer more flexibility and sustainability than government funding, with some foundations providing multi-year commitments to support the long-term growth and development of FQHCs.
Research and identify foundations that align with your mission and funding priorities. Create a grant calendar to keep track of application deadlines, and develop compelling grant proposals that showcase the impact of your programs and services. Network with foundation staff and attend relevant conferences and workshops to learn more about their priorities and application processes.
Example: The California Health Care Foundation (CHCF) has awarded grants to numerous FQHCs, such as the Community Health Partnership in San Jose, to support their programs and services. These grants provide multi-year funding, helping FQHCs maintain stability and plan for the long term.
4. Implement Fee-for-Service Models
While FQHCs are committed to providing care regardless of a patient’s ability to pay, they can still charge fees based on a sliding scale that takes into account the patient’s income and financial situation. By implementing a fee-for-service model, FQHCs can generate revenue while still ensuring that care remains accessible to all patients, regardless of their financial circumstances.
Develop a sliding fee scale policy that aligns with the Health Resources and Services Administration’s (HRSA) guidelines. Train staff to assess patients’ eligibility and collect fees in a compassionate and culturally sensitive manner. Periodically review and adjust the sliding fee scale to reflect changes in the cost of care and the community’s financial circumstances.
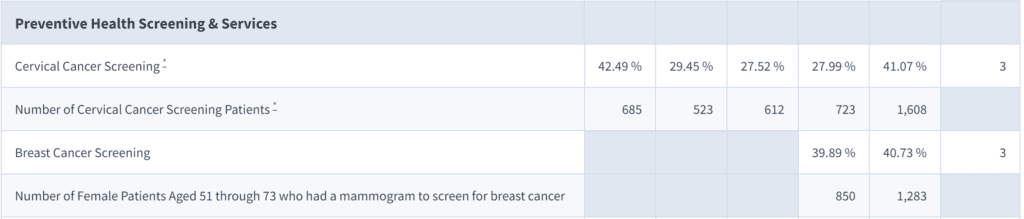
Example: Many FQHCs, such as Cempa Community Health, use a sliding fee scale based on a patient’s income and household size. This allows them to generate revenue while ensuring that care remains accessible to all patients.
Creating a Sliding Scale Fee for FQHCs: A Detailed Guide for FQHCs from Oatmeal Health.
5. Maximize Reimbursement from Public and Private Insurers
FQHCs should work to optimize their billing and reimbursement processes to ensure they receive the maximum possible revenue from public programs like Medicaid and Medicare, as well as private insurance companies. Investing in staff training and technology to streamline billing can result in increased revenue, contributing to the financial stability of the organization.
Conduct a comprehensive review of your billing and reimbursement processes, identifying areas for improvement. Train staff in proper coding and documentation to minimize claim denials and delays. Invest in technology solutions that streamline billing, such as electronic health records (EHRs) and practice management systems.
Example: The Virginia Garcia Memorial Health Center, an FQHC in Oregon, improved its billing and reimbursement processes by investing in staff training and technology. As a result, they experienced increased revenue and reduced administrative costs.
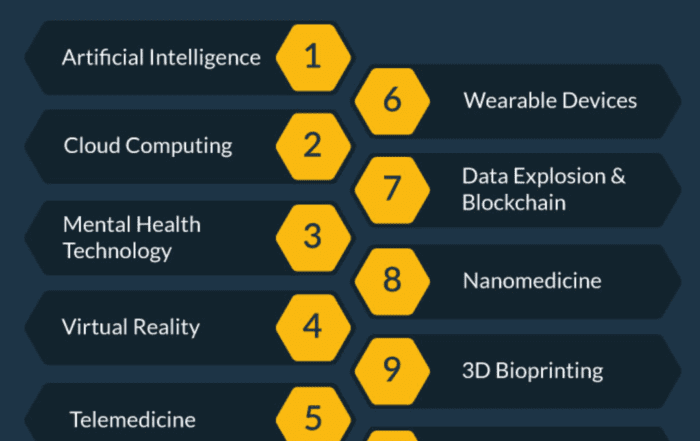
6. Leverage Telehealth and Digital Health Services
The adoption of telehealth and digital health services can help FQHCs increase their reach and generate additional revenue. By offering remote consultations, online health education, and telemonitoring services, FQHCs can attract new patients and create innovative service models that can be reimbursed by insurance providers or offered on a fee-for-service basis.
Assess your organization’s capacity to offer telehealth services, and invest in the necessary technology and infrastructure. Train staff in the use of telehealth platforms and ensure compliance with privacy and security regulations. Develop a marketing strategy to promote your telehealth services to current and potential patients.
Example: In response to the COVID-19 pandemic, Whitman-Walker Health, an FQHC in Washington, D.C., expanded its telehealth services to offer remote consultations, mental health services, and HIV care. This allowed them to continue providing care to their patients while generating revenue.
7. Engage in Social Enterprise
FQHCs can explore opportunities to create social enterprises – businesses that generate revenue while advancing the organization’s social mission. For example, an FQHC might open a pharmacy, dental clinic, or wellness center that offers services to the broader community for a fee. The profits generated by these enterprises can then be reinvested into the FQHC to support its core mission.
Identify potential social enterprise opportunities that align with your mission and have a viable market. Develop a business plan that outlines the goals, strategies, and financial projections for the enterprise. Implement effective marketing and management practices to ensure the success of the enterprise and track its impact on your organization’s financial stability and mission.
Example: The DAP Health, operates a thrift store called Revivals. The revenue generated from the store helps support the clinic’s healthcare services for low-income patients.
8. Collaborate with Other Healthcare Providers and Organizations
Forming partnerships with other healthcare providers and organizations can help FQHCs access new funding opportunities and reduce costs through shared resources and services. By collaborating on joint grant applications, co-hosting events, and engaging in collective advocacy efforts, FQHCs can strengthen their position in the healthcare ecosystem and tap into new sources of support.
Identify potential partners within your local healthcare ecosystem, including hospitals, clinics, and other non-profit organizations. Develop joint projects, grant applications, or advocacy efforts that leverage the unique strengths and resources of each partner. Establish clear communication channels and governance structures to ensure effective collaboration and shared decision-making.
Example: In Oklahoma, Stigler Health and Wellness partnered with a primary care/radiology virtual clinic called Oatmeal Health, that screens their patients for lung cancer using AI and other tech-enabled services, all at no cost to the patient and for the FQHC, fully funded by CMS. These collaborations enable FQHCs to share resources, access new funding opportunities, and advocate for their collective interests.
Conclusion
The reliance on grant funding puts FQHCs at risk of financial instability and can lead to devastating consequences for the patients they serve. To ensure the long-term sustainability of these essential healthcare providers, it is crucial for FQHCs to diversify their funding sources. By implementing strategies such as cultivating partnerships with local businesses, engaging individual donors, maximizing reimbursements from insurers, and exploring social enterprise opportunities, FQHCs can create a more stable financial foundation and continue providing vital healthcare services to vulnerable populations.
A robust and diversified funding strategy is not only beneficial for the FQHCs themselves but also crucial for the health and well-being of the communities they serve.
Share this article and save a life!
Author:

Jonathan is a seasoned executive with a proven track record in founding and scaling digital health and technology companies. He co-founded Oatmeal Health, a tech-enabled Cancer Screening as a Service for Underrepresented patients of FQHCs and health plans, starting with lung cancer. With a strong background in engineering, partnerships, and product development, Jonathan is recognized as a leader in the industry.
Govette has dedicated his professional life to enhancing the well-being of marginalized populations. To achieve this, he has established frameworks for initiatives aimed at promoting health equity among underprivileged communities.
REVOLUTIONIZING CANCER CARE
A Step-by-Step FQHC Guide to Lung Cancer Screening
The 7-page (Free) checklist to create and launch a lung cancer screening program can save your patients’ lives – proven to increase lung cancer screening rates above the ~5 percent national average.
– WHERE SHOULD I SEND YOUR FREE GUIDE? –