Share this article and save a life!
Cancer has destroyed so many lives around the world and it is only getting worse. My father’s prostate cancer just came back a 2nd time and he is undergoing radiation treatment now for the next 8 weeks.
For anyone that is dealing with this firsthand or has family members, it is one of the hardest things to go through, and sadly most of the worst effects of cancer can be mitigated if caught early enough. So why are people not getting screened 100 percent? That is a question for another day.
What Cancers Are More Prevalent?
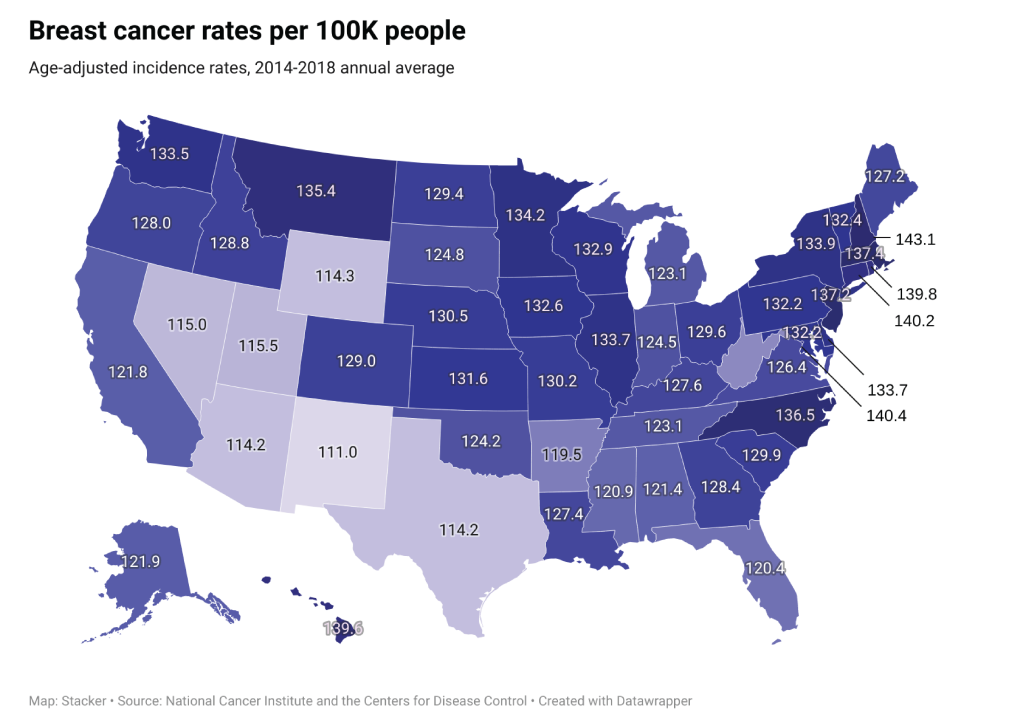
Certain forms of cancer are more common than others, notably in late-stage development. Stacker analyzed cancer incidence data from the National Cancer Institute and CDC to look at where the five most common forms of cancer are most prevalent.
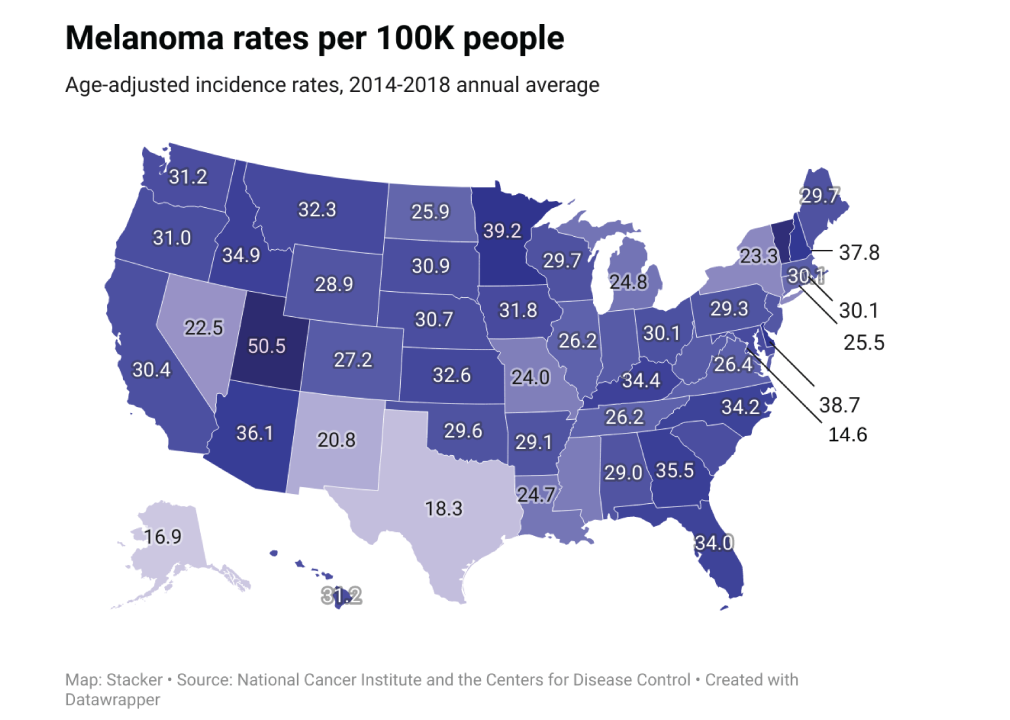
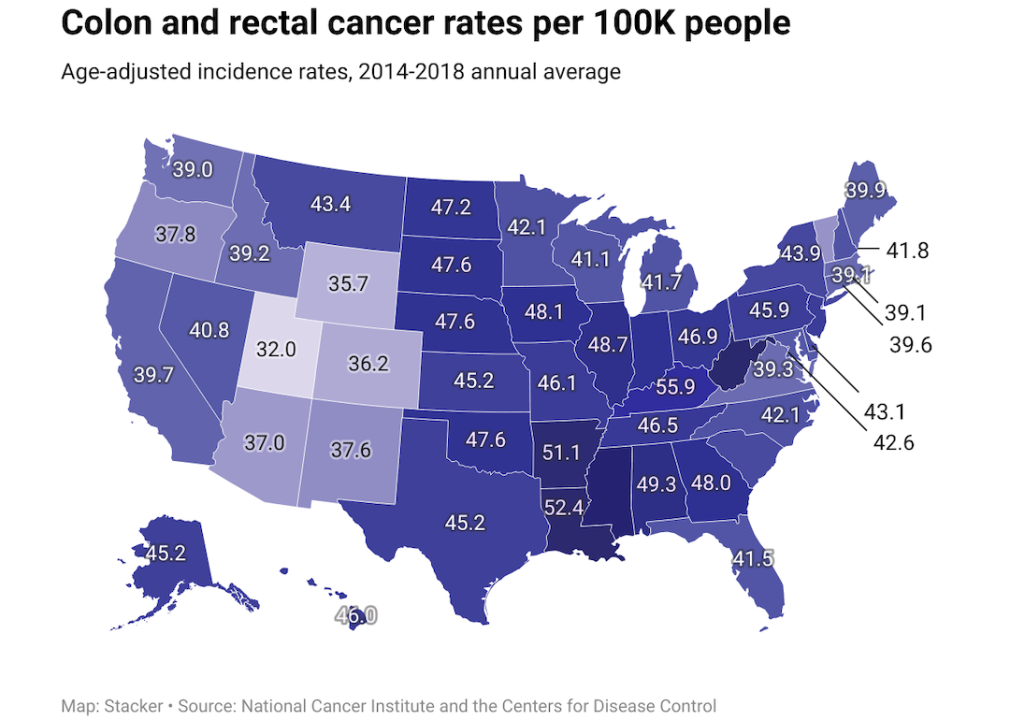
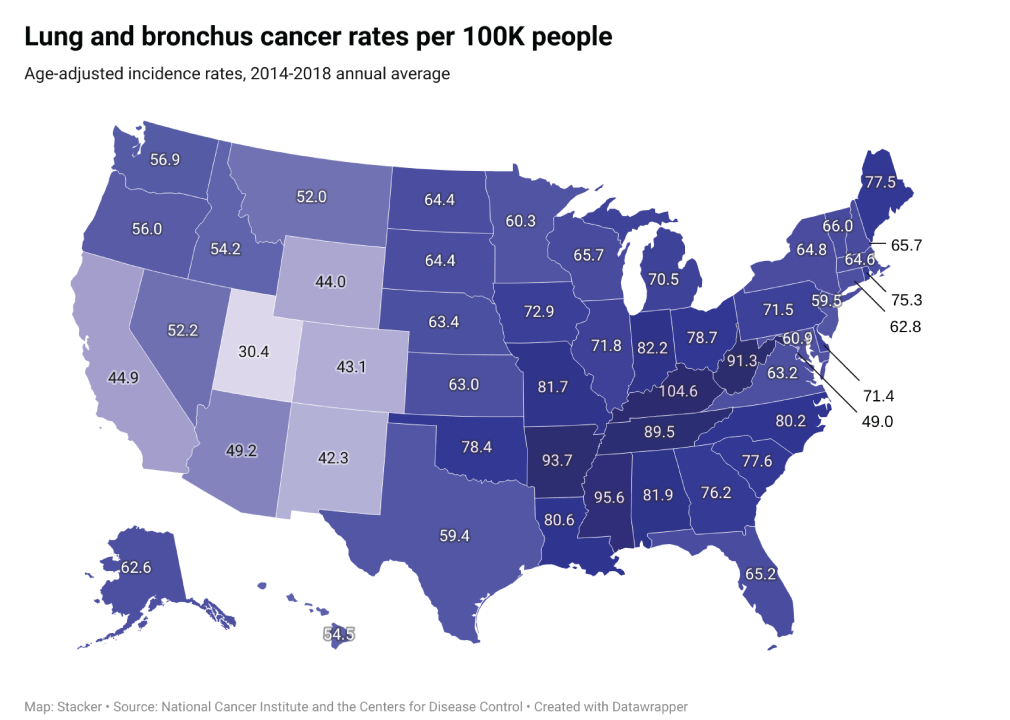
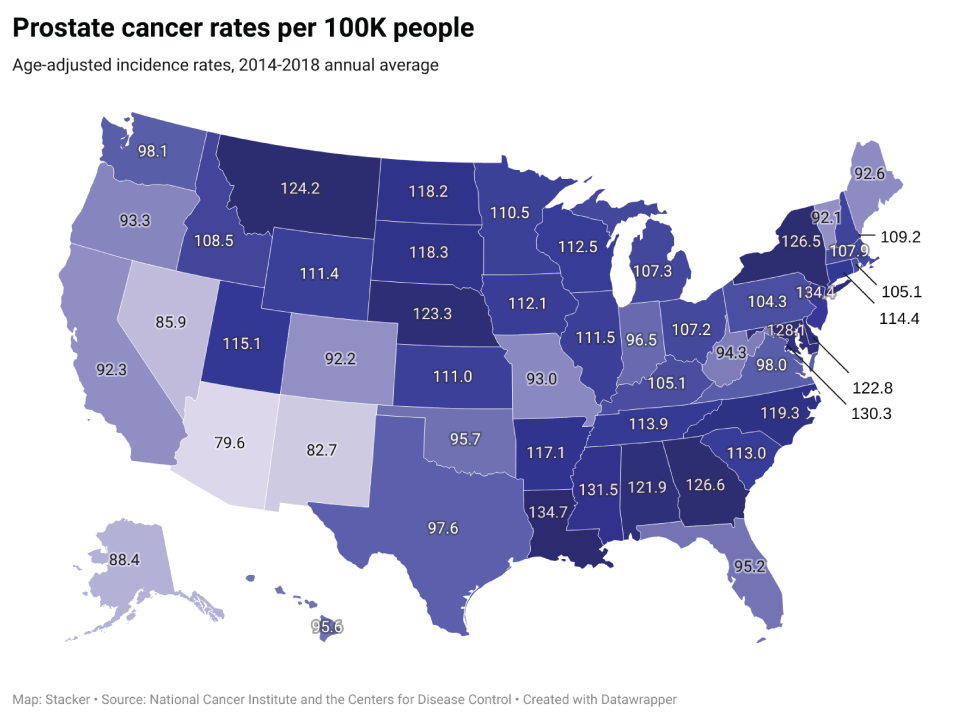
The annual averages in each slide are calculated from data compiled between 2014 and 2018 and have been adjusted for patient age. The data was adjusted to account for the increased likelihood of older people developing cancer, and the state-by-state maps reflect the rates of each type of cancer per 100,000 people.
The following list is derived from the National Institutes of Health’s 2022 projection estimates for the most commonly diagnosed cancers in the U.S., though the projection totals themselves are not included as a data point; a direct comparison would be misleading because this dataset uses compiled and age-adjusted historical data.
Cancer incidence, survival, and mortality rates are population-based indicators of progress against cancer. The mortality-to-incidence ratio can be broadly defined as the percentage of death certificates that include the person’s cancer diagnosis and specify the type of cancer. However, the mortality-to-incidence ratio should not necessarily be interpreted as the survival rate. A cancer diagnosis on a death certificate could have happened at any point in the past and does not necessarily mean the person died of cancer.
Stacker also looked at risk factors for these common cancers, ways to reduce risk, and methods for cancer screening.
You may also like: States with the highest cancer rates
Melanoma
– Average national incidences per year: 49,438
– Percent of incidences in late-stage: 15.0%
– Average annual mortality count: 5,428
— Mortality-to-incidence ratio: 11.0%
The word melanoma means “black tumor.” Its development begins in melanocytes—the cells that produce the pigment melanin. Most people think of melanoma as a type of skin cancer, because it can form in moles on the skin. But it can also form in other pigmented tissues, such as those in the eye or intestine.
Melanoma is less common than other types of skin cancer, but it is more likely than other types of skin cancer to grow and metastasize or spread to other organs. The most common risk factors for melanoma include exposure to ultraviolet light, having many moles or freckles, having lighter hair, and having a family or personal history of melanoma. The use of tanning beds and sun lamps also increases melanoma risk.
The best ways to prevent melanoma are using sunscreen, wearing sun-protective clothing and sunglasses, and seeking shade during midday when the sun is at its strongest.
Colorectal cancer
– Average national incidences per year: 75,374
– Percent of incidences in late-stage: 57.4%
– Average annual mortality count: 27,717
— Mortality-to-incidence ratio: 36.8%
Colorectal cancer develops as malignant cells grow and accumulate in the colon rectum, and usually presents as a growth called a polyp. Risk factors for colorectal cancer include smoking, obesity, age, and family history.
Physical activity, combination hormone replacement therapy, and aspirin reduce the risk of colon cancer. Procedures such as colonoscopy and sigmoidoscopy can find polyps, so the doctor can remove them before they become cancerous. The recommended age for men to begin regular colonoscopies, once 50, is now 45. The fecal occult blood tests screen for blood hidden in the stool, which may be a sign of colorectal cancer.
Lung and bronchus cancer
– Average national incidences per year: 115,218
– Percent of incidences in late-stage: 70.4%
– Average annual mortality count: 78,841
— Mortality-to-incidence ratio: 68.4%
Lung cancer is the third most common kind of cancer in the U.S., according to the NIH, and the leading cause of cancer death in both men and women. Smoking and exposure to secondhand smoke are the most common risk factors associated with lung cancer. Although most cases of lung cancer are caused by smoking, nonsmokers can get lung cancer, too.
There are two types of lung cancer: small-cell lung cancer and non-small-cell lung cancer. The bronchi, the two tubes that lead from the trachea to the lungs, are sometimes also involved in lung cancer. Screening tests for lung cancer are in clinical trials, though LDCT scans have been shown to decrease the risk of death in heavy smokers.
Prostate cancer
– Average national incidences per year: 200,677
– Percent of incidences in late-stage: 20.6%
– Average annual mortality count: 30,566
— Mortality-to-incidence ratio: 15.2%
Prostate cancer is the second most common cancer among men in the U.S. One in eight men in the U.S. will be diagnosed with this type of cancer. The biggest risk factors for prostate cancer are age, race, and family history. It is more common in men over 50, and in Black men compared to white men. Most men diagnosed with prostate cancer do not die of it, because the majority of prostate cancers grow and spread slowly.
Breast cancer
– Average national incidences per year: 249,261
– Percent of incidences in late-stage: 31.9%
– Average annual mortality count: 41,951
— Mortality-to-incidence ratio: 16.8%
Breast cancer is the second most common type of cancer in women in the U.S. It is the second leading cause of cancer death in women, after lung cancer. Older age, a family or personal history of breast cancer, dense breast tissue, obesity, and the use of hormone replacement therapy for the treatment of menopausal symptoms can increase the risk of breast cancer.
Mammography can detect tumors in the breast, even before they have spread to other organs. Mammograms are recommended for women ages 45-54 yearly, and every two years thereafter, except in cases of higher risk factors.
Thanks to Slacker and Kfor.com for the summary.
Share this article and save a life!
Author:

Jonathan Govette is a seasoned healthcare and technology executive with more than two decades of experience building, scaling, and advising digital health companies. He is the Co-Founder and CEO of Oatmeal Health, an AI-driven Lung Cancer Screening and Diagnostics company focused on expanding access to early detection for underrepresented populations, particularly patients served by Federally Qualified Health Centers and value-based health plans.
With a background in engineering, product development, and strategic partnerships, Jonathan has founded and led multiple health technology ventures across clinical care delivery, regulated medical software, and AI-enabled diagnostics. His work sits at the intersection of medicine, technology, and health equity, with a consistent focus on translating complex clinical problems into scalable, real-world solutions.
Jonathan has spent much of his professional life dedicated to improving outcomes for marginalized and underserved communities. He has designed and implemented frameworks that align clinical quality, reimbursement, and technology to sustainably advance health equity at scale. This mission is deeply personal and informs his leadership philosophy and long-term vision for healthcare transformation.
In addition to his operating experience, Jonathan is an author and long-time writer in the healthcare domain, with over 20 years of published work covering digital health, medical innovation, and healthcare systems. He is a frequent mentor to early-stage founders and regularly advises startups on product strategy, partnerships, and go-to-market execution in regulated healthcare environments.
Before entering industry full-time, Jonathan nearly pursued a career in medicine with an early path toward cardiothoracic surgery, an experience that continues to shape his clinical perspective and respect for frontline care delivery.
CEO | Oatmeal Health | AI Lung Cancer Startup | Engineer | Writer | Almost Became a Doctor (Cardiac Thoracic Surgeon) | 3x Health Tech Founder | Startup Mentor | Follow to share what I’ve learned along the way.